NUR223absection 4 Maternity Final Exam
ATI NUR223absection 4 Maternity Final Exam
Total Questions : 99
Showing 10 questions Sign up for moreExplanation
D. A distended bladder can displace the uterus, causing the fundus to deviate from the midline. This deviation is due to the bladder pushing the uterus to one side, which interferes with uterine contraction and can lead to complications like uterine atony and excessive bleeding.
A. Frequent uterine contractions are normal in the immediate postpartum period as the uterus contracts to reduce in size (involution). These contractions help control bleeding and aid in returning the uterus to its pre-pregnancy state. While uterine contractions are expected, they do not directly indicate bladder distention.
B. Lochia is the vaginal discharge that occurs after childbirth, progressing through stages (rubra, serosa, alba) over several weeks. A small amount of rubra lochia (bright red, indicating recent bleeding) on the perineal pad suggests minimal postpartum bleeding, which is a normal finding. However, it does not directly indicate bladder distention.
C. Increased thirst can occur postpartum due to fluid shifts, hormonal changes, and breastfeeding. While hydration status is important, increased thirst alone does not directly indicate bladder distention.
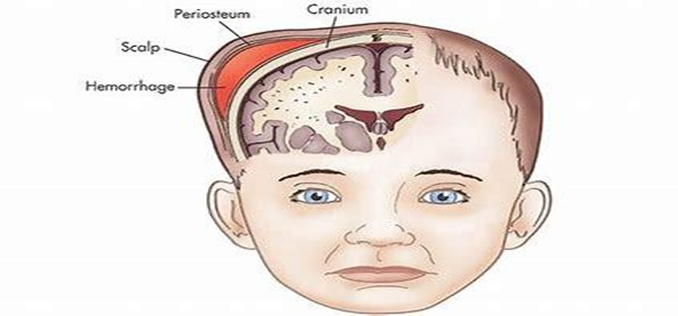
The nurse is performing a newborn assessment and evaluates a collection of blood beneath the newborn's scalp that does not cross the suture lines. The nurse documents this finding as
Explanation
D. Cephalohematoma is another condition seen in newborns involving the collection of blood beneath the periosteum of the infant's skull bones. Unlike caput succedaneum, cephalohematoma does not cross suture lines because it is confined by the edges of a single cranial bone.
A. Sinciput refers to the anterior part of the fetal skull. It is not a term used to describe any specific condition or abnormality of the newborn scalp.
B. Occiput posterior refers to the position of the baby's head during labor and delivery, where the back of the baby's head (occiput) is towards the mother's posterior pelvis. It does not describe a scalp condition.
C. Caput succedaneum is a common condition in newborns characterized by swelling or edema of the scalp that crosses suture lines. It typically occurs due to pressure against the mother's cervix or vaginal wall during labor. The swelling is fluid collection beneath the scalp skin and often resolves within a few days without treatment.
Explanation
A. Rh immunoglobulin is given to Rh-negative mothers during and after pregnancy to prevent them from developing Rh antibodies against Rh-positive red blood cells. Without RhIG, Rh-negative mothers may develop antibodies if they are exposed to Rh-positive fetal blood (such as during delivery or other pregnancy-related events), which could lead to complications in future pregnancies.
B. Rh immunoglobulin is not given to prevent Rh antibodies in Rh-positive newborns; rather, it prevents Rh-negative mothers from developing antibodies against Rh-positive fetal red blood cells.
C. Rh immunoglobulin does not destroy Rh antibodies in newborns. It prevents the mother's immune system from producing these antibodies in the first place, thereby protecting future pregnancies from HDFN.
D. Rh immunoglobulin does not destroy existing Rh antibodies in Rh-negative mothers. Instead, it works prophylactically by binding to and neutralizing Rh-positive fetal red blood cells that may have entered the maternal circulation, thus preventing the mother from developing Rh antibodies.
Explanation
A. During breastfeeding, it's important for the newborn to take not only the nipple but also a portion of the surrounding areola into their mouth. Placing both the nipple and some of the areola ensures that the baby can latch deeply onto the breast. A deep latch helps the baby effectively extract milk, stimulates milk flow, and reduces the risk of nipple pain or damage.
B. Newborns do have innate reflexes that help them find and latch onto the breast but their latch can still benefit from proper positioning and guidance from the mother. Encouraging the mother to understand how to position the nipple and areola correctly can enhance the breastfeeding experience for both the mother and baby.
C. It may not be necessary to emphasize placing breast tissue beyond the areola into the baby's mouth. The key focus should be on ensuring that the nipple and a significant portion of the areola are taken into the baby's mouth to achieve a deep latch.
D. Even though a newborn's mouth is small, effective breastfeeding depends on achieving a deep latch, which involves taking both the nipple and some of the areola into the mouth. Encouraging the mother to aim for only part of the nipple could lead to shallow latch, ineffective milk transfer, and potential nipple soreness.
Explanation
B. A sudden gush of clear fluid from the vagina, especially if it continues to leak, is a classic sign that the amniotic sac has ruptured, known as the rupture of membranes or "water breaking." This can occur as a sign of early labor, although it does not always mean active labor has begun. It is important for the client to notify their healthcare provider if this occurs.
A. Sharp, right-sided abdominal pain is not typically associated with the beginning signs of labor. It could indicate other conditions such as appendicitis or gallbladder issues, which would require medical evaluation. Therefore, this option is not correct in the context of signs of labor.
C. An increased pulse rate and upper abdominal pain can be signs of certain complications during pregnancy but they are not typical signs of the onset of labor itself. These symptoms could indicate conditions such as preeclampsia or other medical issues that need prompt evaluation by a healthcare provider.
D. Excessive fatigue and headache can occur during pregnancy due to hormonal changes, increased physical demands, or other factors. However, they are not specific signs of the onset of labor. These symptoms should be discussed with a healthcare provider to determine their cause and appropriate management.
Explanation
B. Auscultation of fetal heart tones is typically best achieved over the fetal back. In this case, the nurse palpated a long, smooth surface on the client's right side, indicating the fetal back is on the right. Therefore, the nurse should expect to auscultate fetal heart tones in the right upper quadrant of the maternal abdomen where the back is located.
A. Typically not where fetal back and heart tones would be auscultated.
C. Unlikely as the fetal back was felt on the right side.
D. Too general without specifying the location relative to fetal positioning.
E. Not consistent with the fetal back being on the right side.
Explanation
D. Newborns delivered by cesarean section are at increased risk of respiratory distress due to incomplete drainage of lung fluid, delayed lung expansion, or other factors related to the delivery process. Respiratory distress may present as grunting, flaring of nostrils, retractions (visible pulling in of the chest wall), or cyanosis (blue discoloration) of the skin.
A. Accidental lacerations are a concern but are less likely immediately following a scheduled cesarean delivery where the procedure is controlled and sterile. They would typically be addressed after more critical assessments are completed.
B. Acrocyanosis refers to the bluish discoloration of the hands and feet, which is common in newborns and usually resolves on its own. While it is important to note, especially for documentation and ongoing assessment, it is not typically an immediate priority unless accompanied by other signs of respiratory or circulatory compromise.
C. Hypothermia, or low body temperature, is a significant concern in newborns because they are vulnerable to heat loss. Newborns delivered by cesarean section are at higher risk of hypothermia due to exposure to a cooler environment and delayed skin-to-skin contact. Maintaining the newborn's temperature through drying, warm blankets, and skin-to-skin contact with the mother is crucial to prevent hypothermia.
Explanation
B. Changing the client's position can help improve fetal oxygenation by relieving pressure on the inferior vena cava and improving blood flow to the placenta.
A. Applying a fetal scalp electrode can provide more accurate and continuous monitoring of the fetal heart rate. However, it is not the first action to take when late decelerations are noted.
C. Increasing IV fluid rate may be considered if hypovolemia or dehydration is suspected as contributing factors to late decelerations. However, it is not typically the first action taken unless there are signs of maternal hypotension or inadequate fluid intake.
D. Administering oxygen can help improve fetal oxygenation and is generally indicated for late decelerations. However, changing the client's position to improve uteroplacental perfusion is typically prioritized over oxygen administration.
Explanation
A. Hypotension is a common side effect of epidural opioid analgesia due to sympathetic blockade. This can lead to decreased placental perfusion and fetal distress. Therefore, a low blood pressure reading such as 80/56 mm Hg is a priority finding that requires immediate nursing intervention. The nurse should assess for signs of hypotension (e.g., dizziness, pallor, decreased urine output) and implement measures to improve blood pressure
B. Pruritus (itching) is a common side effect of opioid analgesia due to its effect on histamine release. While uncomfortable for the client, it is generally not life-threatening or an immediate priority unless it becomes severe and affects the client's ability to breathe or is accompanied by other symptoms such as rash or difficulty swallowing.
C. A temperature elevation (fever) can indicate infection, which is important to monitor during labor. However, a single temperature reading of 38.2°C (100.8°F) alone may not be immediately alarming, especially if the client is not exhibiting other signs of infection such as chills, increased uterine tenderness, or foul-smelling vaginal discharge. It should be further assessed, but it is not typically the highest priority compared to hypotension.
D. Motor weakness in the lower extremities can occur with epidural analgesia due to the effects of local anesthetics or opioids on nerve function. While it should be addressed, especially to prevent falls or injury to the client, it is not as immediately concerning as hypotension, which can compromise maternal and fetal well-being.
Explanation
D. This condition often indicates that the bladder is full, which can push the uterus out of its normal position. A full bladder can also inhibit the uterus from contracting properly, which is crucial to prevent excessive bleeding. By urinating, the client can help the uterus return to its proper position and continue to contract effectively to maintain hemostasis.
A. Urinary catheterization is typically done if the client is unable to urinate spontaneously and has a distended bladder, which isn't indicated by the assessment findings.
B. Massaging the fundus helps to ensure that it remains firm, which promotes uterine involution and helps to prevent postpartum hemorrhage. However, if the urinary bladder is not emptied, the action may not be effective.
C. Administering an analgesic may be necessary if the client is experiencing pain, but it is not the priority action based on the assessment findings provided. The displaced fundus and its firmness are more concerning in terms of immediate postpartum care.
You just viewed 10 questions out of the 99 questions on the ATI NUR223absection 4 Maternity Final Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



