Custom maternity exam #2 2024
ATI Custom maternity exam #2 2024
Total Questions : 57
Showing 10 questions Sign up for moreA nurse is collecting data from a postpartum client.
Which of the following findings should alert the nurse to the possibility of a postpartum complication?
Explanation
Choice A rationale:
The fundus at the umbilicus level is a normal finding in the immediate postpartum period. After delivery, the top of the uterus
(known as the fundus) is typically at the level of the umbilicus. In the days following delivery, the uterus begins to shrink and
descend into the pelvic cavity, guided by the process known as involution.
Choice B rationale:
A urinary output of 3,000 mL is unusually high and could indicate a postpartum complication. Postpartum diuresis is common
as the body eliminates excess fluid accumulated during pregnancy. However, excessive urinary output could be a sign of
postpartum complications such as postpartum preeclampsia, which can occur after the birth of the baby and is characterized
by high blood pressure and signs of damage to another organ system, often the kidneys.
Choice C rationale:
A temperature of 100.4 F for two days postpartum can be a normal finding. It’s not uncommon for women to experience a
slight elevation in temperature in the first 24 hours after delivery due to the exertion of labor. However, a temperature above100.4 F beyond the first 24 hours could indicate an infection and should be evaluated.
Choice D rationale:
A cesarean section shortly following delivery is not typically a sign of a postpartum complication. It’s a surgical procedure used to deliver the baby and can be planned or unplanned due to various reasons such as the baby’s position, multiple pregnancies, or complications during labor. However, like any surgery, a cesarean section does carry risks and can increase the likelihood of certain postpartum complications such as infection or blood clots.
A nurse is assisting with the care of a client who is in labor and has the urge to push.
Which of the following instructions should the nurse give the client?
Explanation
Choice A rationale:
Pushing continuously throughout the entire contraction can lead to maternal exhaustion and may not be the most effective way to progress labor. It’s important for the mother to conserve her energy and work with her body’s natural rhythms.
Choice B rationale:
Taking a deep, cleansing breath before and after each contraction can help the mother manage pain and keep her energy up.
This technique is often recommended because it allows the mother to rest briefly and gather strength for the next contraction.

Choice C rationale:
While it’s important for the nurse to monitor contractions and provide guidance, the urge to push is a natural response that
can vary among individuals. Telling the mother when to push according to contractions may not align with her body’s natural
instincts.
Choice D rationale:
Holding one’s breath and pushing while someone counts to ten is an outdated practice. This method can cause unnecessary
strain and doesn’t take into account the individual rhythms and responses of the mother’s body.
Which of the following findings should the nurse monitor to evaluate the effectiveness of this medication?
Explanation
Choice A rationale:
Oxytocin is a hormone that causes the uterus to contract. It is often given to women after childbirth to help the uterus return
to its normal size and to prevent heavy bleeding. Therefore, monitoring the consistency of the fundus (the upper part of the
uterus) is an effective way to evaluate the effectiveness of this medication.
Choice B rationale:
While urinary output is an important vital sign to monitor in all patients, it is not directly related to the effectiveness of
Oxytocin. Oxytocin does not have a significant effect on urinary output.
Choice C rationale:
Blood pressure is another vital sign that should be monitored in all patients. However, it is not the primary indicator of
Oxytocin’s effectiveness. While Oxytocin can cause blood pressure changes, these are usually transient and not the primary
intended effect of the medication.
Choice D rationale:
Heart rate, like blood pressure and urinary output, is an important vital sign to monitor in all patients. However, it is not the
primary indicator of Oxytocin’s effectiveness. Oxytocin does not have a significant direct effect on heart rate.
A nurse is assisting with the care of a client who is in labor.
The client's labor is difficult and prolonged and she reports a severe backache.
Which of the following factors is a contributing cause of difficult, prolonged labor?
Explanation
Choice A rationale:
Fetal attitude in general flexion is not a contributing factor to difficult, prolonged labor. In fact, it is the normal fetal attitude
during labor. The fetus is typically in a position of general flexion, where the head is flexed forward, chin to chest, and the arms
and legs are flexed, with the arms crossed over the chest and the legs bent at the knees.
Choice B rationale:
Fetal lie being longitudinal is the normal and most common fetal lie during labor. In a longitudinal lie, the long axis of the fetus
is parallel with the long axis of the mother. This is the ideal and most common position for labor and delivery.
Choice C rationale:
A gynecoid pelvis is the most common type of female pelvis and is the most favorable for childbirth. It has a round shape with
a wide pubic arch, which allows for easier passage of the baby during delivery.
Choice D rationale:
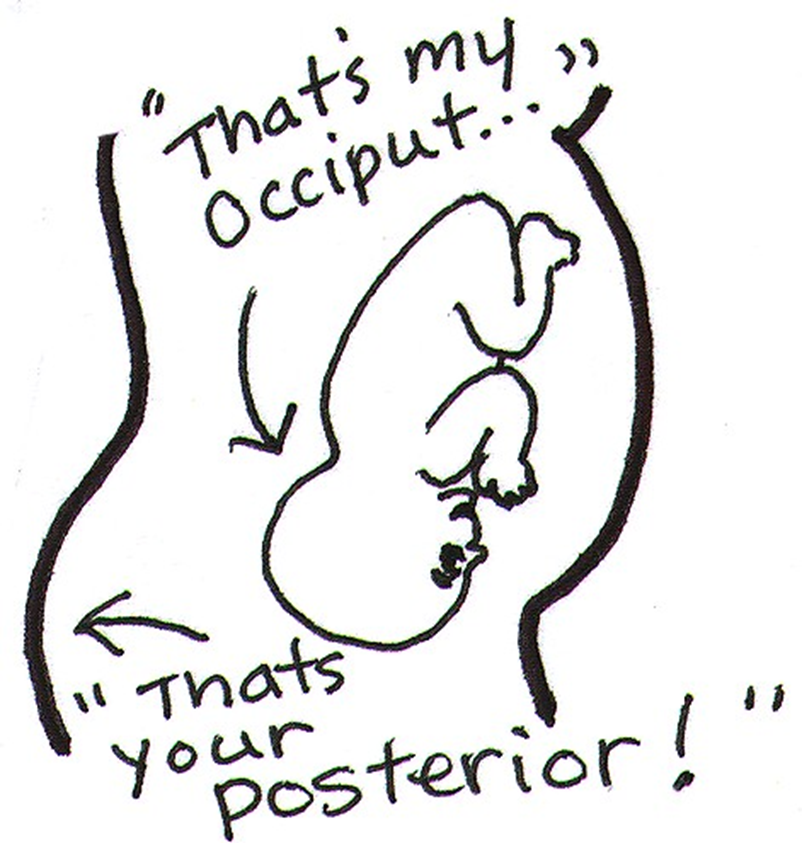
A persistent occiput posterior (OP) position can indeed contribute to difficult, prolonged labor. In an OP position, the baby’s
occipital bone is towards the mother’s posterior side. This position can cause labor to be more painful and last longer because the baby’s head diameter that presents to the birth canal is larger. It can also cause back pain during labor, often referred to as "back labor"1.
Which of the following actions should the nurse take first?
Explanation
Choice A rationale:
Checking the client’s blood pressure is important, but it is not the first action the nurse should take. Hypotension could
indicate hemorrhage, but the nurse needs to address the immediate risk of excessive bleeding.
Choice B rationale:
The nurse should first massage the client’s fundus. A saturated perineal pad could indicate a postpartum hemorrhage.
Massaging the fundus helps the uterus contract and may stop the bleeding.
Choice C rationale:
Observing for pooling of blood under the buttocks is a way to assess for bleeding. However, this is not the first action because
it does not address the cause of the bleeding.
Choice D rationale:
Administering oxytocin can help the uterus contract and reduce bleeding. However, this is not the first action because it
requires a physician’s order.
breastfeeding her newborn.
Which of the following client statements indicates an understanding of the teaching?
Explanation
Choice A rationale:
Stopping breastfeeding until the antibiotics are done is not a recommended practice. Most antibiotics are safe to use while
breastfeeding. Moreover, stopping breastfeeding can lead to engorgement.
Choice B rationale:
Applying cold compresses 20 minutes before each feeding is not a recommended practice. Cold compresses are usually
recommended after breastfeeding to help reduce swelling. Warm compresses or taking a warm shower before breastfeeding
can help increase milk flow and promote the letdown reflex.
Choice C rationale:
Feeding the baby every 2 hours is a good practice to prevent breast engorgement. Frequent feeding helps to empty the breasts,
which can prevent them from becoming overly full and engorged.
Choice D rationale:
Not wearing a bra during the daytime is not a recommended practice. Wearing a well-fitted bra can provide support and help
reduce discomfort associated with breast engorgement.
The nurse observes the umbilical cord protruding from the vagina.
Which of the following actions should the nurse take first?
Explanation
Choice A rationale:
Preparing the client for an emergency cesarean birth is an important step, but it is not the first action the nurse should take.
The immediate priority is to relieve pressure on the cord to prevent or alleviate cord compression.
Choice B rationale:
Covering the cord with a sterile, moist saline dressing is done to prevent drying of the cord and to maintain blood flow.
However, this is not the first action to take. The priority is to relieve cord compression by changing the client’s position.
Choice C rationale:
While it is important to explain to the client what is happening, this should not be the first action. The nurse’s priority is to
ensure the safety of the mother and baby, which involves immediate interventions to relieve cord compression.
Choice D rationale:
Placing the client in a knee-chest or Trendelenburg position is the first action the nurse should take. This position helps to
reduce pressure on the cord, which can improve blood flow to the fetus. It is a critical intervention that can prevent serious
complications such as fetal hypoxia.
The nurse finds a small amount of lochia rubra on the client's perineal pad, and the fundus is midline and firm at the
umbilicus.
Which of the following actions should the nurse take?
Explanation
Choice A rationale:
Assisting the client to ambulate is not the immediate action required in this scenario. The nurse has found a small amount of
lochia rubra on the client’s perineal pad, and the fundus is midline and firm at the umbilicus. These are normal findings for a
client who is 4 hours postpartum. However, the nurse should ensure that there is no excessive bleeding, which could be a sign
of postpartum hemorrhage.
Choice B rationale:
Performing a fundal massage is not necessary in this case. Fundal massage is usually performed when the uterus is boggy or
soft, which could indicate uterine atony, a leading cause of postpartum hemorrhage. In this scenario, the fundus is firm and at
the level of the umbilicus, which is a normal finding 4 hours postpartum.
Choice C rationale:
Increasing the rate of IV fluids is not the immediate action required in this scenario. IV fluids are usually increased to expand
intravascular volume in cases of postpartum hemorrhage. In this case, the nurse has found a small amount of lochia rubra on
the client’s perineal pad, which is a normal finding 4 hours postpartum.
Choice D rationale:
Checking for blood under the client’s buttocks is the correct action for the nurse to take in this scenario. This is to ensure that
there is no excessive bleeding, which could be hidden under the client’s buttocks. Excessive bleeding could be a sign of
postpartum hemorrhage, a potentially life-threatening complication.
A nurse is assisting in the care of a client who is in the second stage of labor.
Which of the following findings should the nurse report to the provider?
Explanation
Choice A rationale:
The presence of a “bloody show” from the vagina is a normal part of labor. It’s caused by the expulsion of the mucus plug that
has sealed the cervix during pregnancy. This is a common occurrence and does not need to be reported to the provider.
Choice B rationale:
Early decelerations in the Fetal Heart Rate (FHR) are usually not a cause for concern. They are often a sign of head
compression, which is a normal occurrence during labor. Therefore, this finding does not need to be reported to the provider.
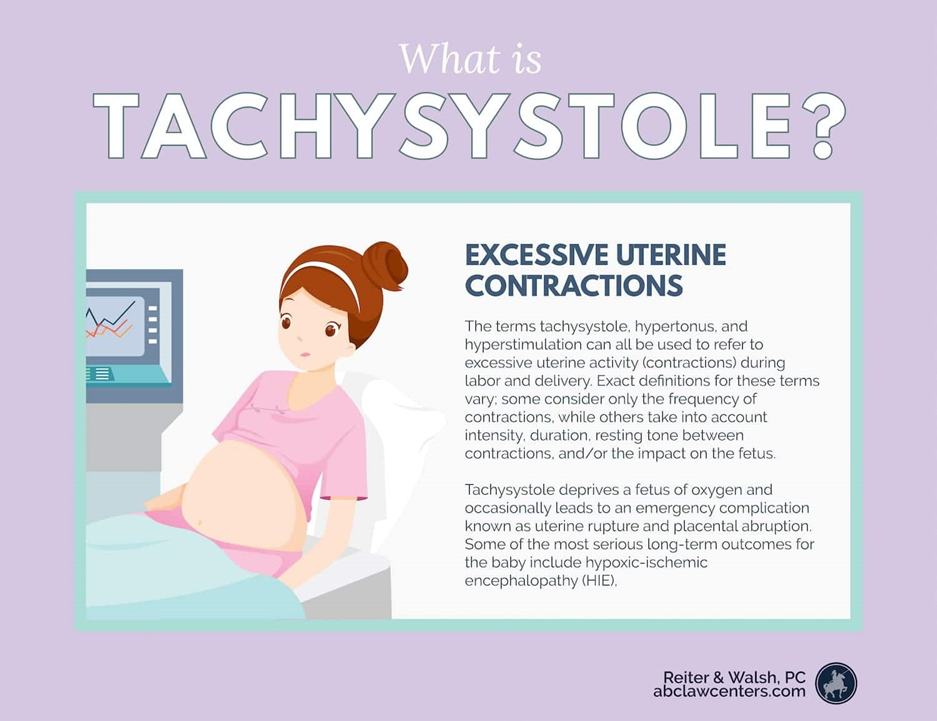
Choice C rationale:
Uterine contractions lasting 2 minutes could be a sign of a complication known as “uterine tachysystole” or “hyperstimulation”. This condition can reduce oxygen supply to the baby and may require medical intervention. Therefore, this finding should be reported to the provider.
Choice D rationale:
Feeling pelvic pressure with contractions is a normal part of the second stage of labor. This pressure is due to the baby moving
down into the birth canal. Therefore, this finding does not need to be reported to the provider.
A nurse is assisting a client who is postpartum with her first breastfeeding experience.
When the client asks how much of the nipple she should put into the baby's mouth, which of the following responses
by the nurse is appropriate?
Explanation
Choice A rationale:
When breastfeeding, it’s important for the baby to latch onto not just the nipple, but also some of the areola, which is the
darker circle of skin around the nipple. This allows the baby to get a deep latch, which is necessary for effective breastfeeding.
The baby’s chin should be firmly touching the breast, and their mouth should be wide open. When they attach, you should see
much more of the darker nipple skin above the baby’s top lip than below their bottom lip.
Choice B rationale:
While it’s true that babies have certain instincts when it comes to breastfeeding, they still need guidance and proper
positioning to latch correctly. Simply relying on the baby’s instincts may not ensure a proper latch, which could lead to
ineffective breastfeeding and potential discomfort for the mother.
Choice C rationale:
The size of the baby’s mouth does not determine how much of the nipple they should take in. Regardless of the size of the
baby’s mouth, they should still latch onto the nipple and some of the areola for effective breastfeeding. Taking only part of the
nipple could lead to a shallow latch, which can cause nipple pain and may not allow the baby to get enough milk.
Choice D rationale:
While it’s important for the baby to take in a good amount of the breast tissue, including the nipple and areola, during
breastfeeding, suggesting to include some breast tissue beyond the areola might be excessive. The key is to ensure a deep
latch, which typically involves the nipple and some of the areola, rather than the entire areola and additional breast tissue.
You just viewed 10 questions out of the 57 questions on the ATI Custom maternity exam #2 2024 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



