A nurse is assisting in the care of a client who is in the second stage of labor.
Which of the following findings should the nurse report to the provider?
Bloody show from the vagina
Early decelerations in the FHR
Uterine contraction lasting 2 minutes
Pelvic pressure with contractions
The Correct Answer is C
Choice A rationale:
The presence of a “bloody show” from the vagina is a normal part of labor. It’s caused by the expulsion of the mucus plug that
has sealed the cervix during pregnancy. This is a common occurrence and does not need to be reported to the provider.
Choice B rationale:
Early decelerations in the Fetal Heart Rate (FHR) are usually not a cause for concern. They are often a sign of head
compression, which is a normal occurrence during labor. Therefore, this finding does not need to be reported to the provider.
Choice C rationale:
Uterine contractions lasting 2 minutes could be a sign of a complication known as “uterine tachysystole” or “hyperstimulation”. This condition can reduce oxygen supply to the baby and may require medical intervention. Therefore, this finding should be reported to the provider.
Choice D rationale:
Feeling pelvic pressure with contractions is a normal part of the second stage of labor. This pressure is due to the baby moving
down into the birth canal. Therefore, this finding does not need to be reported to the provider.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A rationale:
Uterine atony is the most common cause of postpartum hemorrhage, and it is characterized by a lack of uterine muscle tone,
which leads to excessive bleeding after delivery.
A macrosomic newborn (weighing over 4000 g) is a significant risk factor for uterine atony because the overdistention of the
uterus during pregnancy can impair its ability to contract effectively after delivery.
Other risk factors for uterine atony include prolonged labor, multiple gestations, rapid labor, use of oxytocin or magnesium
sulfate during labor, and a history of uterine atony in previous deliveries.
It's crucial for a nurse to closely monitor clients with these risk factors for signs of uterine atony, such as excessive vaginal
bleeding, a soft and boggy uterus, and a rising fundus.
Prompt recognition and management of uterine atony are essential to prevent life-threatening hemorrhage.
Choice B rationale:
Retained placental fragments can also contribute to postpartum hemorrhage; however, they are not as strongly associated
with macrosomia as uterine atony.
Risk factors for retained placental fragments include premature separation of the placenta, placenta accreta, and manual
removal of the placenta.
Choice C rationale:
Thrombophlebitis, a blood clot formation in a vein, is a postpartum complication, but it's not directly related to macrosomia.
Risk factors for thrombophlebitis include venous stasis, hypercoagulability, and trauma to the veins, such as from prolonged
bed rest or cesarean delivery.
Choice D rationale:
Perineal infection is also a potential postpartum complication, but it's not specifically linked to macrosomia.
Risk factors for perineal infection include perineal lacerations, episiotomy, and poor hygiene.
Correct Answer is D
Explanation
Choice A rationale:
Rh positive individuals already have the Rh factor on their red blood cells, so they do not need Rho(D) immune globulin to
prevent sensitization.
The newborn being Rh positive does not pose a risk to an Rh positive mother, as their blood types are compatible.
Choice B rationale:
Rh positive individuals cannot develop antibodies against the Rh factor, as it is already present on their own red blood cells.
The newborn's Rh negative status does not create a risk of sensitization for the mother, as there is no Rh factor to trigger an
immune response.
Choice C rationale:
If both the mother and the newborn are Rh negative, there is no risk of Rh incompatibility.
This is because neither individual has the Rh factor on their red blood cells, so there is no potential for sensitization.
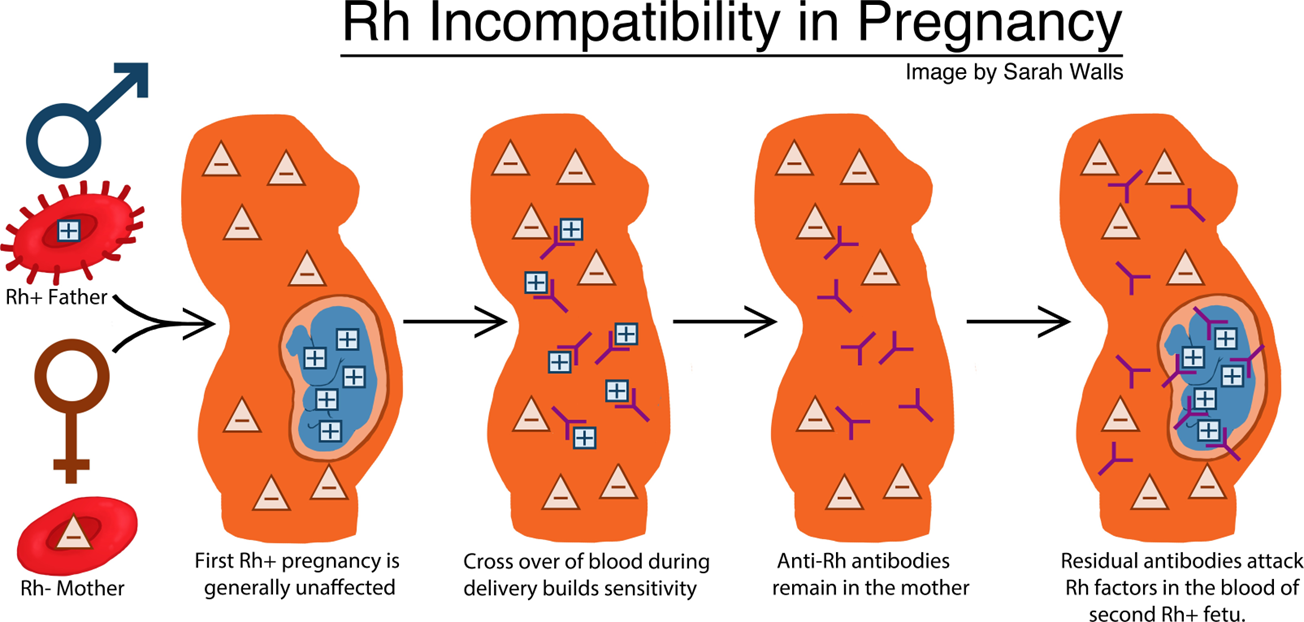
Choice D rationale:
When an Rh negative mother carries an Rh positive fetus, there is a risk of Rh sensitization during pregnancy and delivery.
This occurs when fetal blood cells cross the placenta and enter the mother's bloodstream, exposing her immune system to the
Rh factor.
If the mother's immune system recognizes the Rh factor as foreign, it can produce antibodies against it.
These antibodies can cross the placenta in subsequent pregnancies and attack the red blood cells of Rh positive fetuses,
leading to hemolytic disease of the newborn (HDN).
Rho(D) immune globulin is a medication that can prevent Rh sensitization by binding to Rh positive fetal blood cells that have
entered the mother's bloodstream.
This prevents the mother's immune system from recognizing the Rh factor and producing antibodies.
Rho(D) immune globulin is typically given to Rh negative mothers within 72 hours of delivery of an Rh positive newborn, as well as after other events that could lead to Rh sensitization, such as miscarriage, abortion, or ectopic pregnancy.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
