A nurse is caring for a client who is postpartum.
Which of the following findings is an indication for the nurse to administer Rho(D) immune globulin?
The client is Rh positive and the newborn is Rh positive
The client is Rh positive and the newborn is Rh negative
The client is Rh negative and the newborn is Rh negative
The client is Rh negative and the newborn is Rh positive
The Correct Answer is D
Choice A rationale:
Rh positive individuals already have the Rh factor on their red blood cells, so they do not need Rho(D) immune globulin to
prevent sensitization.
The newborn being Rh positive does not pose a risk to an Rh positive mother, as their blood types are compatible.
Choice B rationale:
Rh positive individuals cannot develop antibodies against the Rh factor, as it is already present on their own red blood cells.
The newborn's Rh negative status does not create a risk of sensitization for the mother, as there is no Rh factor to trigger an
immune response.
Choice C rationale:
If both the mother and the newborn are Rh negative, there is no risk of Rh incompatibility.
This is because neither individual has the Rh factor on their red blood cells, so there is no potential for sensitization.
Choice D rationale:
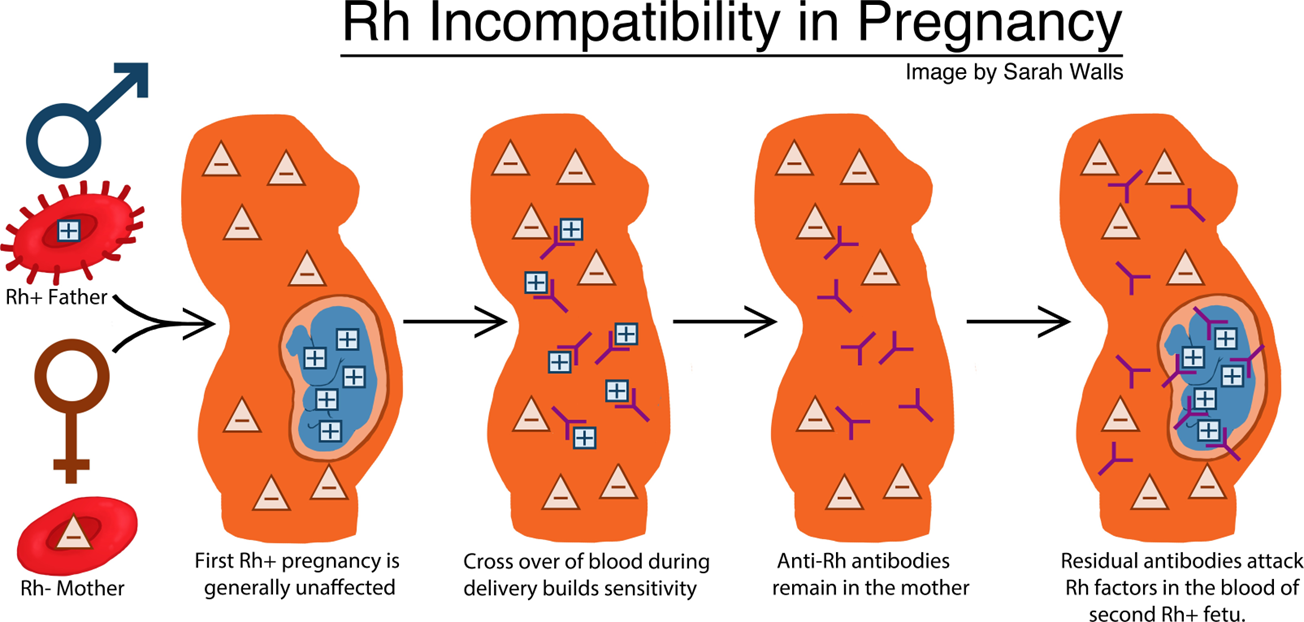
When an Rh negative mother carries an Rh positive fetus, there is a risk of Rh sensitization during pregnancy and delivery.
This occurs when fetal blood cells cross the placenta and enter the mother's bloodstream, exposing her immune system to the
Rh factor.
If the mother's immune system recognizes the Rh factor as foreign, it can produce antibodies against it.
These antibodies can cross the placenta in subsequent pregnancies and attack the red blood cells of Rh positive fetuses,
leading to hemolytic disease of the newborn (HDN).
Rho(D) immune globulin is a medication that can prevent Rh sensitization by binding to Rh positive fetal blood cells that have
entered the mother's bloodstream.
This prevents the mother's immune system from recognizing the Rh factor and producing antibodies.
Rho(D) immune globulin is typically given to Rh negative mothers within 72 hours of delivery of an Rh positive newborn, as well as after other events that could lead to Rh sensitization, such as miscarriage, abortion, or ectopic pregnancy.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A rationale:
Fever: A hallmark sign of inflammation, fever is a common and often early manifestation of endometritis. The body's
thermostat, located in the hypothalamus, is reset to a higher temperature in response to infection or inflammation. This
triggers a cascade of physiological events, including chills, shivering, and increased heat production, as the body attempts to
fight off pathogens. In endometritis, the fever is typically 100.4°F (38°C) or higher.
Chills: Often accompanying fever, chills are a sensation of coldness despite a normal or elevated body temperature. They result
from involuntary muscle contractions, which generate heat in an attempt to raise the body's temperature. Chills can be mild or
severe, and they often precede a rise in temperature.
Choice B rationale:
Increased heart rate: Tachycardia, or an increased heart rate, can occur in endometritis, but it is not a specific finding. It can be
present in various other conditions, including anxiety, pain, dehydration, anemia, and other infections. While it may be a sign
of endometritis, it's not considered a primary manifestation.
Choice C rationale:
Lower abdominal pain: Lower abdominal pain is a common symptom in postpartum women, but it is not always indicative of
endometritis. It can result from uterine contractions, incisional pain (if a cesarean section was performed), bladder distention,
constipation, or other postpartum complications. While it may be present in endometritis, it's not a specific finding.
Choice D rationale:
Unusual vaginal discharge: Lochia, the normal postpartum vaginal discharge, can vary in color and amount. However, unusual
vaginal discharge, such as foul-smelling or purulent discharge, can be a sign of endometritis. It's important to note that not all
women with endometritis will have abnormal discharge.
Correct Answer is D
Explanation
Choice A rationale:
Placing pillows under the client's knees can actually increase the risk of thrombophlebitis. This is because it flexes the knees,
which can cause blood to pool in the legs. This pooling of blood can lead to the formation of blood clots.
Choice B rationale:
Keeping the client on bed rest is also a risk factor for thrombophlebitis. This is because immobility can cause blood to pool in
the legs. It's important to encourage early and frequent ambulation to promote venous return and prevent clot formation.
Choice C rationale:
Applying warm, moist soaks to the client's lower legs can help to relieve the symptoms of thrombophlebitis, but it does not
prevent it. Warm compresses can help to improve circulation and reduce inflammation, but they're not a preventative
measure.
Choice D rationale:
Encouraging the client to ambulate frequently is the most effective way to prevent thrombophlebitis. This is because it helps to
promote venous return and prevent blood from pooling in the legs. Ambulation also helps to activate the calf muscles, which
act as a natural pump to help move blood back to the heart.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
