RN Maternal Newborn 2023
RN Maternal Newborn 2023
Total Questions : 63
Showing 10 questions Sign up for moreA nurse is caring for a newborn Immediately following birth.
Exhibit 1
The nurse is assessing the newborn 24 hr later. How should the nurse interpret the findings?
For each finding, click to specify whether the finding is unrelated to the diagnosis, an indication that the client's condition is Improving, or an Indication that the client's condition is worsening.
Explanation
A nurse is caring for a client who is at 12 weeks of gestation and has hyperemesis gravidarum.
The nurse is assessing the client 24 hr later. How should the nurse interpret the findings?
For each finding click to specify whether the finding is unrelated to the diagnosis, a sign of potential improvement, or a sign of potential worsening condition.
Explanation
For the findings 24 hours later, the nurse should interpret them as follows:
Urinary output: 40 ml/hr
Interpretation: Sign of potential worsening condition
Explanation: A urinary output of 40 ml/hr is concerning and indicates potential dehydration. It is a sign of potential worsening of the client's condition, as it suggests inadequate fluid intake or ongoing fluid losses.
3+ ketones
Interpretation: Sign of potential worsening condition
Explanation: The presence of 3+ ketones in the urine suggests ongoing ketosis, which can occur in hyperemesis gravidarum due to starvation and the breakdown of fats for energy. It is a sign of potential worsening of the client's nutritional status.
Heart rate: 100/min
Interpretation: Sign of potential improvement
Explanation: A heart rate of 100/min is within the normal range. It can be interpreted as a sign of potential improvement, indicating that the client's cardiovascular system is maintaining an appropriate heart rate.
WBC count: 10,000/mm3
Interpretation: Unrelated to diagnosis
Explanation: The WBC count within the normal range (10,000/mm3) is unrelated to the diagnosis of hyperemesis gravidarum. It does not provide specific information about the client's condition in this context.
Urine specific gravity: 1.050
Interpretation: Sign of potential worsening condition
Explanation: A urine specific gravity of 1.050 is elevated and indicates concentrated urine. This finding is a sign of potential worsening of the client's dehydration status.
Urine pH: 5
Interpretation: Unrelated to diagnosis
Explanation: The urine pH of 5 is within the normal range and is unrelated to the diagnosis of hyperemesis gravidarum. It does not provide specific information about the client's condition in this context.
A nurse is caring for a newborn who was born at 39 weeks of gestation and is 36hr old.
Which of the following findings should the nurse report to the provider?
Select all that apply
Explanation
In the context of the newborn's information, the nurse should report the following findings to the provider:
A. Coombs test result:
Explanation: The Coombs test checks for the presence of antibodies that can destroy red blood cells. In the absence of information about any specific concern or risk factors, a Coombs test result may not be immediately necessary for a term newborn. The nurse should report this finding to the provider for clarification on why the test was performed.
D. Intake and output:
Explanation: The newborn has voided only once since birth. Infrequent voiding can be a concern, and the nurse should report this to the provider for further evaluation, as adequate urine output is important to assess renal function and hydration status.
G. Mucous membrane assessment:
Explanation: Mucous membrane color and moisture are important indicators of hydration. If there are abnormalities, such as pale or dry mucous membranes, the nurse should report this to the provider for further assessment.
H. Sclera color:
Explanation: The color of the sclera can indicate jaundice in a newborn. If the sclera color appears yellow or jaundiced, the nurse should report this finding to the provider for further evaluation.
The following findings are not typically of immediate concern in the given context:
B. Glucose level:
Explanation: While glucose levels are important in certain situations, there is no information suggesting a need for immediate concern about glucose levels in this case. The nurse can monitor blood glucose levels as part of routine care but does not need to report it without specific concerns.
C. Head assessment finding:
Explanation: The information does not provide details about any abnormal head assessment findings. If there are no specific concerns mentioned, the nurse may not need to report this finding unless there are abnormalities observed during routine assessments.
E. Respiratory rate:
Explanation: The respiratory rate is not highlighted as a concern in the given information. If there are no specific abnormalities or signs of respiratory distress, the nurse may not need to report this finding without additional information.
F. Heart rate:
Explanation: The heart rate is not highlighted as a concern, and a normal Apgar score was noted at 5 minutes. If there are no specific concerns or abnormal findings related to the heart rate, the nurse may not need to report this finding without additional information.
A nurse is caring for a client who is at 32 weeks of gestation and has complete placenta previa
Which of the following assessment findings requires immediate follow-up)
Select all that apply
Explanation
In the context of a client at 32 weeks of gestation with complete placenta previa, the following assessment findings require immediate follow-up:
A. Fetal heart rate:
Explanation: An elevated fetal heart rate (174/min) may be indicative of fetal distress. This finding requires immediate follow-up to assess the well-being of the fetus.
F. Vaginal bleeding:
Explanation: A moderate amount of bright red vaginal bleeding is a concerning sign, especially in the context of complete placenta previa. It indicates active bleeding, and immediate follow-up is necessary to assess the severity of the situation and the well-being of both the mother and the fetus.
C & D. Hemoglobin (Hgb) and Hematocrit (Hct):
Explanation: Hemoglobin and hematocrit levels are important indicators of blood loss. Given the vaginal bleeding, these values need immediate follow-up to assess the extent of maternal blood loss and the potential need for blood transfusion.
The following assessment findings do not require immediate follow-up in the given context:
B. Fundal height:
Explanation: Fundal height (33cm) is typically measured to assess fetal growth. While it's important to monitor, it may not be an immediate concern unless there are other signs of fetal distress.
E. Platelet count:
Explanation: While platelet count is important, it may not require immediate follow-up unless there is evidence of severe bleeding and a potential risk of disseminated intravascular coagulation (DIC). In this scenario, attention to Hgb and Hct is more urgent.
G & H. White Blood Cell (WBC) count and Red Blood Cell (RBC) count:
Explanation: WBC count and RBC count may be monitored but do not require immediate follow-up unless there are signs of infection or other complications not evident in the given information.
A nurse is caring for a term newborn who is 48 hr old
The nurse assessing the newborn 24 hr later. How should the nurse interpret the findings?
For each finding, click to specify whether the finding is unrelated to the diagnosis, a sign of potential improvement, or a sign of potential worsening condition.
Explanation
Transient strabismus:
Interpretation: Unrelated to diagnosis
Explanation: Transient strabismus (crossed eyes) is not necessarily related to the maternal history of opioid use or precipitous birth. It is a common finding in newborns and often resolves on its own without intervention.
Respiratory rate 70/min:
Interpretation: Sign of potential worsening condition
Explanation: A respiratory rate of 70/min in a newborn is higher than the normal range (30-60 breaths per minute). This could indicate respiratory distress, infection, or other complications, requiring further assessment.
Continuous high-pitched cry:
Interpretation: Sign of potential worsening condition
Explanation: A continuous high-pitched cry can be a sign of potential distress or discomfort in a newborn. It may be associated with various conditions, including withdrawal symptoms related to maternal opioid use during pregnancy. This finding warrants further assessment.
Regurgitation:
Interpretation: Unrelated to diagnosis
Explanation: Regurgitation (spitting up) is a common occurrence in newborns and is not necessarily related to the maternal history of opioid use. It is often a normal physiological process in infants.
Loose stools:
Interpretation: Unrelated to diagnosis
Explanation: Loose stools can be a normal finding in newborns and may not be directly related to the maternal history of opioid use. It is not necessarily indicative of a worsening condition in this context.
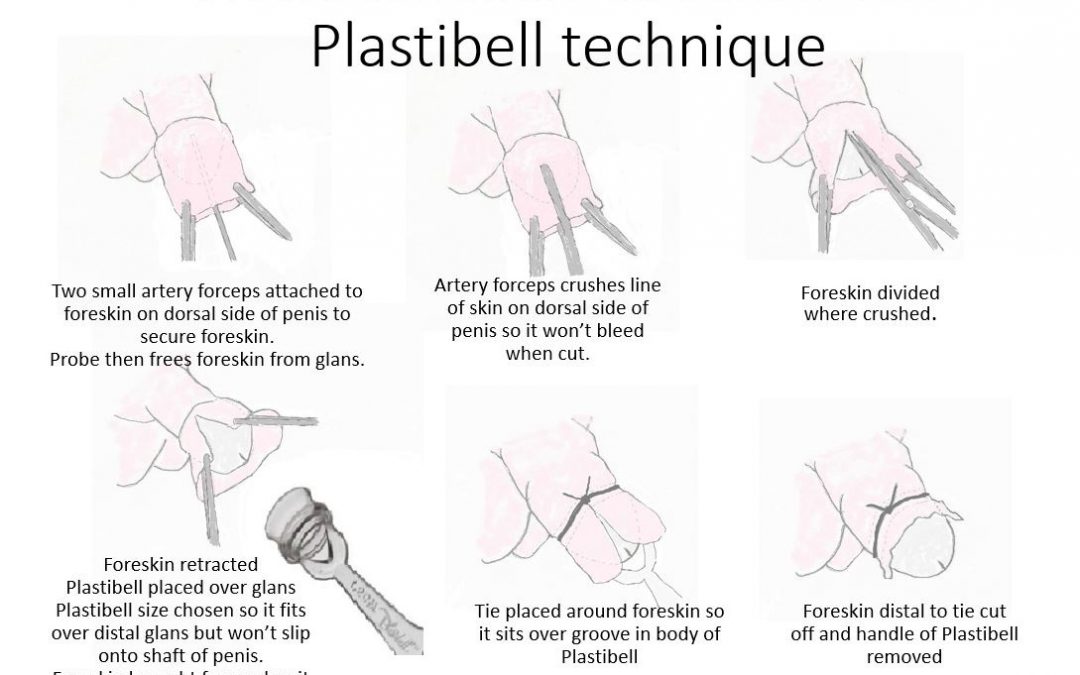
A nurse is providing teaching to the parents of a newborn about the Plastibell circumcision technique. Which of the following information should the nurse include?
Explanation
A.It is normal for a yellow exudate to form at the surgical site within 24 hours after a Plastibell circumcision.This is part of the healing process and should not be mistaken for an infection.
B.The Plastibell device is not removed manually.It typically falls off on its own within 7 to 10 days.
C.The diaper should be loose to avoid pressure on the circumcised area, which can cause discomfort and delay healing.
D.It is normal for the area around the Plastibell to darken as the tissue dies and the ring prepares to fall off.However, parents should notify the provider if there are signs of infection, excessive bleeding, or if the Plastibell does not fall off within the expected time frame.
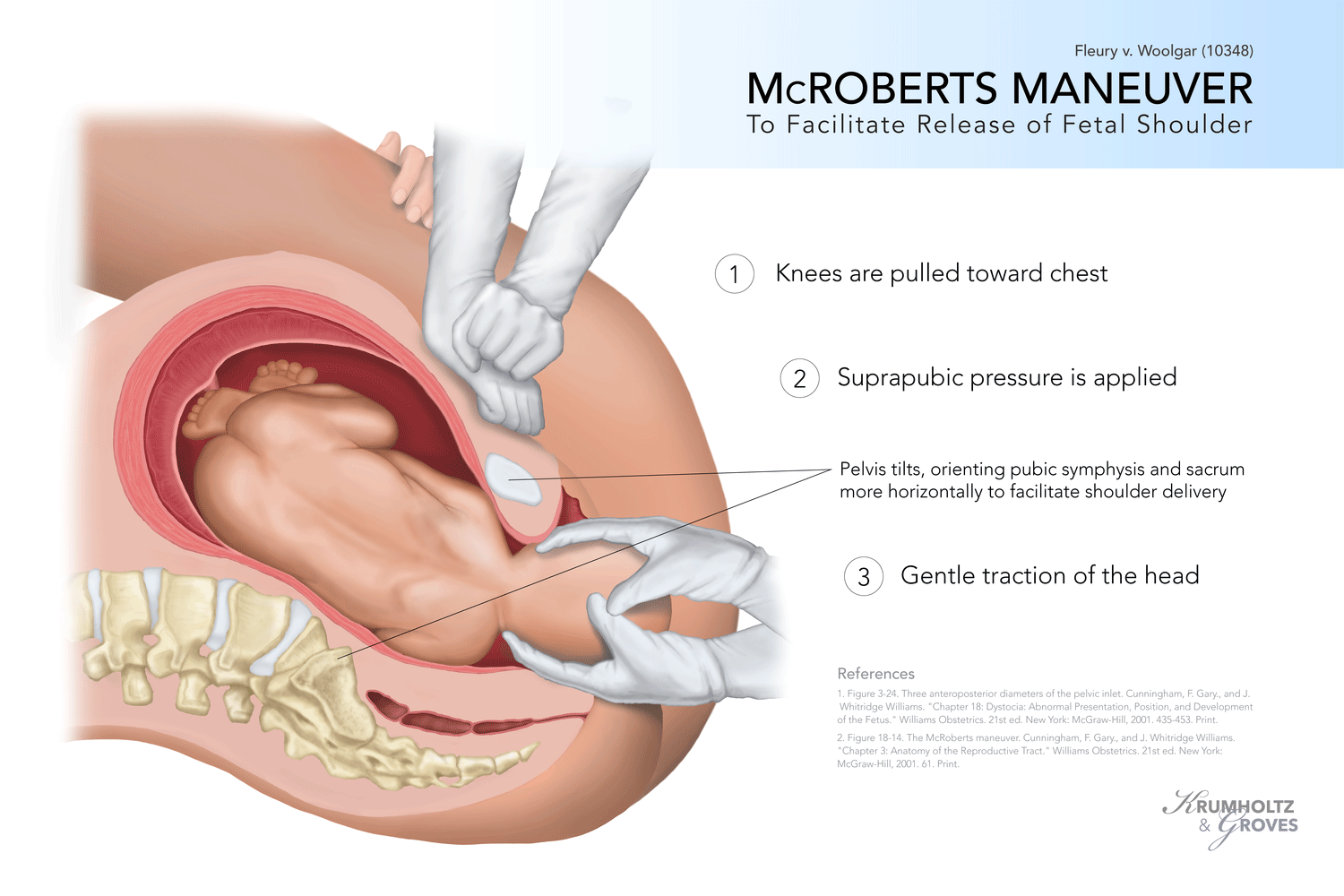
A nurse is caring for a client who is in the second stage of labor and is experiencing a shoulder dystocia. The provider instructs the nurse to perform the McRoberts maneuver. Which of the following actions should the nurse take?
Explanation
A. Move the client onto their hands and knees: This position is often used for the Gaskin maneuver, which involves positioning the mother on all fours to help resolve shoulder dystocia. However, the McRoberts maneuver specifically requires hyperflexing the legs toward the abdomen.
B. Press firmly on the client’s suprapubic area: This action is not part of the McRoberts maneuver. It is not the recommended technique for resolving shoulder dystocia.
C. Assist the client in pulling their knees toward their abdomen
The McRoberts maneuver involves hyperflexing the mother's legs toward her abdomen to widen the pelvic outlet. This repositions the pelvis, which can assist in dislodging the impacted shoulder of the baby during a shoulder dystocia.
D. Apply pressure to the client’s fundus: Applying pressure to the fundus can sometimes be used in other obstetric emergencies but is not part of the McRoberts maneuver for shoulder dystocia.
A nurse is providing teaching about the expected effects of magnesium sulfate to a client who is at 28 weeks of gestation and has preeclampsia. Which of the following responses by the nurse is appropriate?
Explanation
A. This medication increases cardiac output: Magnesium sulfate does not typically increase cardiac output. Its primary role in the context of preeclampsia is to prevent seizures and manage hypertension.
B. This medication stabilizes the fetal heart rate: While magnesium sulfate can have a relaxing effect on the uterus, which might indirectly influence fetal heart rate, its primary purpose in preeclampsia is seizure prevention rather than fetal heart rate stabilization.
C. The medication improves tissue perfusion: Magnesium sulfate primarily functions as an anticonvulsant and tocolytic (relaxes the uterus). While its effects on vasodilation can contribute to improved blood flow, the primary indication in preeclampsia is seizure prevention.
D. The medication prevents seizures
Magnesium sulfate is commonly used in the management of preeclampsia to prevent seizures (eclampsia), a serious complication of the condition. It has anticonvulsant properties and is the primary medication for seizure prophylaxis in pregnant individuals with preeclampsia.
A nurse is caring for a client who delivered by cesarean birth 6 hr ago. The nurse notes a steady trickle of vaginal bleeding that does not stop with fundal message. Which of the following actions should the nurse take?
Explanation
A. Administer 500 ml lactated Ringer's IV bolus:
This choice may be relevant in the context of postpartum hemorrhage, but the first step should be to assess the client's status, including urinary output. Administering fluids without a clear assessment may not address the underlying cause.
B. Replace the surgical dressing:
Vaginal bleeding after a cesarean birth is unlikely to be addressed by replacing the surgical dressing. This action may not address the root cause of the bleeding, which needs further assessment.
C. Apply an ice pack to the incision site:
Using an ice pack is not the appropriate intervention for postpartum bleeding. Ice is typically used for pain and swelling, not for controlling bleeding.
D. Evaluate urinary output:
This is the correct choice. Evaluating urinary output is crucial to assess the client's overall fluid status and kidney perfusion. In the context of postpartum bleeding, it helps determine if there is hypovolemia or other issues contributing to the bleeding. Adequate urinary output is a positive sign of organ perfusion.
A nurse is providing teaching to a postpartum client who has a prescription for a rubella immunization. Which of the following client statements indicates understanding of the teaching?
Explanation
A. I will receive a series of three immunizations, and each one will be a month apart: This statement is not accurate for rubella immunization. The MMR vaccine is usually administered as a single injection.
B. I should avoid becoming pregnant for at least 1 month following the immunization
Rubella immunization is typically administered as the measles, mumps, and rubella (MMR) vaccine. The statement indicating understanding reflects awareness of the importance of avoiding pregnancy for a certain period after receiving the rubella immunization due to potential risks to the developing fetus.
C. I should avoid breastfeeding for 2 weeks following the immunization: Breastfeeding is not a contraindication after receiving the rubella immunization. In fact, breastfeeding is generally not affected, and mothers can continue to breastfeed.
D. I will report joint pain that develops after the immunization to my provider immediately: Joint pain is a potential side effect of the rubella vaccine. Reporting joint pain to the provider is essential for monitoring and addressing any adverse reactions.
You just viewed 10 questions out of the 63 questions on the RN Maternal Newborn 2023 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



