RN HESI OB/pediatrics
RN HESI OB/pediatrics
Total Questions : 44
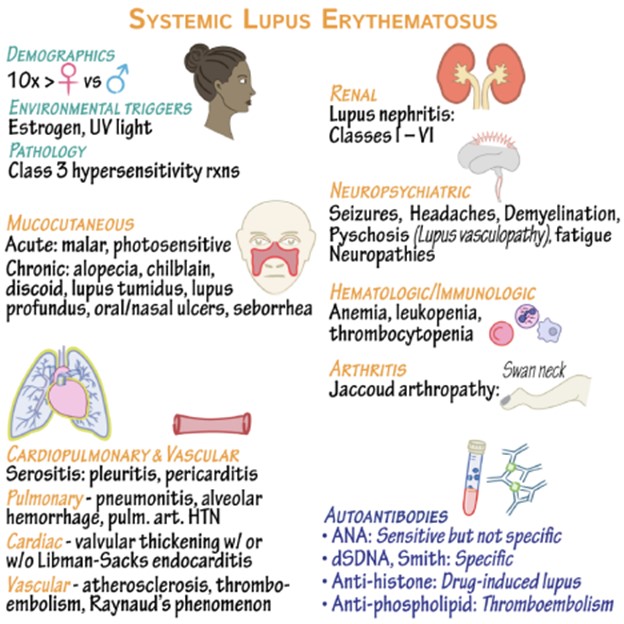
Showing 10 questions Sign up for moreThe nurse caring for a client with systemic lupus erythematosus (SLE) would include which information in teaching about triggers that can result in an exacerbation of the disease?
Explanation
Excessive exposure to UV light, such as sunlight or tanning beds, is a known trigger for SLE exacerbations. It is important for individuals with SLE to protect their skin from the sun by wearing protective clothing, using sunscreen, and avoiding direct sunlight during peak hours. Having a family history of SLE increases the risk of developing the disease. While it is not a trigger in itself, it is an important piece of information for the client to be aware of, as it may indicate a genetic predisposition to the condition.
Acetaminophen is a commonly used over-the-counter pain reliever. While it can help manage pain associated with SLE, it is not typically considered a trigger for exacerbations. Menopause, which marks the end of a woman's reproductive years, does not directly trigger SLE exacerbations. However, hormonal changes during menopause can potentially affect disease activity in some individuals. It is important for the client to discuss any changes or concerns with their healthcare provider to manage their symptoms effectively.
A patient, age 23, underwent a rhinoplasty 6 hours ago. After administering his pain medication, the nurse notes that he is swallowing frequently. What is the most likely cause of the swallowing?
Explanation
Rhinoplasty is a surgical procedure performed on the nose, and it often involves the placement of nasal packing to control bleeding, support the nasal structures, and promote healing. Nasal packing can cause mouth breathing and oral dryness, which can lead to increased swallowing as the patient tries to alleviate the discomfort.
While bleeding posterior to the nasal packing is a potential complication of rhinoplasty, it typically presents with other symptoms such as active bleeding, nasal discharge, or changes in vital signs. Without additional information or signs of active bleeding, it is less likely to be the cause of the patient's frequent swallowing in this scenario.
An adverse reaction to the analgesic is possible, but it would typically present with other symptoms such as allergic reactions (rash, swelling, difficulty breathing) or gastrointestinal symptoms (nausea, vomiting). In the absence of these symptoms, an adverse reaction to the analgesic is less likely.
Lastly, a normal response to the analgesic and surgery would not typically manifest as frequent swallowing. While pain medication can cause side effects, such as drowsiness or nausea, increased swallowing is not a common response.
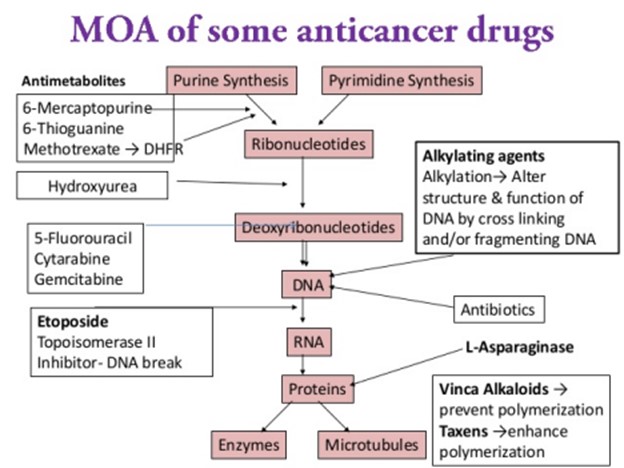
A 58-year-old man is going to have chemotherapy for lung cancer. He asks the nurse how the chemotherapeutic drugs will work.The most accurate explanation the nurse can give is which of the following?
Explanation
Chemotherapy is a treatment modality used to target and destroy rapidly dividing cells, including cancer cells. It works by interfering with the cell division process, which is a characteristic of cancer cells. However, it is important to note that chemotherapy drugs can also affect normal, healthy cells in the body that undergo rapid division, such as cells in the bone marrow, hair follicles, and gastrointestinal lining. This is why chemotherapy can be associated with side effects like bone marrow suppression, hair loss, and gastrointestinal disturbances. While the molecular structure of DNA can be altered by certain chemotherapeutic drugs, this explanation is not comprehensive enough to encompass the overall mechanism of action of chemotherapy.
The statement that "cancer cells are susceptible to drug toxins" is partially true, as cancer cells are generally more vulnerable to the cytotoxic effects of chemotherapy drugs compared to normal cells.
Chemotherapy aims to disrupt the division and growth of cancer cells rather than promoting their division.
A patient with a gastric outlet obstruction has been treated with NG decompression. After the first 24 hours, the patient develops nausea and increased upper abdominal bowel sounds. What is the best action by the nurse?
Explanation
The development of nausea and increased upper abdominal bowel sounds after 24 hours of NG decompression in a patient with gastric outlet obstruction raises concerns for possible complications or changes in the patient's condition. Assessing the patient's vital signs, including blood pressure, heart rate, respiratory rate, and oxygen saturation, can provide important information about their circulatory status and overall stability.
While checking the patency of the NG tube is important, it is not the best immediate action in this situation. The nurse should first assess the patient's vital signs to ensure their stability before proceeding with further interventions.
Placing the patient in a recumbent position (lying down) or encouraging deep breathing and conscious relaxation may not address the underlying issue and could potentially exacerbate the symptoms. It is essential to assess the patient's vital signs and circulatory status to determine the appropriate course of action.
A client with systemic lupus erythematosus (SLE) is receiving nonsteroidal anti- inflammatory drug (NSAID) therapy. Which side effect of NSAID therapy should the nurse immediately report to the health care provider?
Explanation
Pancytopenia refers to a decrease in all three major blood cell types: red blood cells (anemia), white blood cells (leukopenia), and platelets (thrombocytopenia). It is a potentially serious side effect that can lead to increased susceptibility to infections, anemia-related symptoms (fatigue, weakness), and an increased risk of bleeding. Prompt reporting is necessary for further
evaluation and appropriate management.
While melena (dark, tarry stools) is a concerning side effect, it typically indicates gastrointestinal bleeding, which should also be reported promptly but may not require immediate action unless the bleeding is severe or accompanied by other symptoms.
Decreased vision can be a side effect of certain medications, including NSAIDs, but it does not usually require immediate reporting unless it is severe or rapidly progressive. Hyperglycemia (high blood sugar) can occur with NSAID therapy, especially in individuals with preexisting diabetes or impaired glucose tolerance. While it should be monitored and managed appropriately, it does not typically require immediate reporting unless it is extremely high or associated with other concerning symptoms.
The nurse determines that teaching for the patient with peptic ulcer disease has been effective when the patient makes which statement?
Explanation
Effective teaching for a patient with peptic ulcer disease focuses on promoting understanding and adherence to the treatment plan, as well as addressing lifestyle modifications that can help manage the condition. Stress reduction is an important aspect of ulcer management, as stress
can exacerbate symptoms and delay healing. If the patient acknowledges learning relaxation strategies that decrease their stress, it indicates that they have grasped the concept and are likely to implement it in their daily life.
It is crucial for the patient to understand that any potential side effects should be reported to the healthcare provider, who will then determine the appropriate course of action. Abruptly stopping medications without medical guidance can have adverse consequences. While pain relief is an important goal, the treatment for peptic ulcer disease typically involves addressing the underlying cause, such as Helicobacter pylori infection or reducing stomach acid production. The patient should follow the treatment regimen as prescribed by the healthcare provider, even if they experience pain relief, to ensure proper healing and prevent ulcer recurrence.
Different antacids have different formulations and ingredients, and they may vary in terms of effectiveness and duration of action. It is important for the patient to consult with their healthcare provider or pharmacist to determine which antacid is most suitable for their specific needs.
The nurse is caring for a patient with COPD. Which intervention could be delegated to unlicensed assistive personnel (UAP)?
Explanation
Assisting the patient to get out of bed is a task that can be safely delegated to UAP, as long as the patient's mobility and transfer status allow for assistance without the need for specialized nursing skills. UAPs are trained to provide basic patient care, including assisting with activities of daily living, under the supervision and direction of licensed healthcare professionals.
Teaching the patient to purse lip breath requires knowledge and understanding of the technique, as well as the ability to assess the patient's response and provide feedback. This is best done by a licensed healthcare professional, such as a nurse or respiratory therapist. Auscultating breath sounds every 4 hours requires the ability to correctly use a stethoscope and interpret the findings. This task falls within the scope of practice of a nurse or respiratory therapist who has received appropriate training.
Planning patient activities to minimize exertion requires knowledge of the patient's condition, limitations, and goals. It involves assessment, evaluation, and coordination of care, which are typically performed by licensed healthcare professionals.
Which medication should the nurse anticipate being used first in the emergency department for relief of severe respiratory distress related to asthma?
Explanation
Albuterol is a short-acting beta-agonist bronchodilator that provides rapid relief of bronchospasm and helps to alleviate the symptoms of respiratory distress in asthma. It acts quickly to relax the smooth muscles in the airways, improving airflow and relieving wheezing, coughing, and shortness of breath. In an acute asthma exacerbation, albuterol is often the first-line medication used to provide immediate relief and improve respiratory function. Prednisone is an oral corticosteroid that has anti-inflammatory effects and is commonly used in the treatment of asthma. However, it is typically administered orally and takes time to exert its effects. In the emergency department setting, the focus is on providing immediate relief of symptoms, and oral medications like prednisone may not have an immediate effect. Ipratropium is an anticholinergic bronchodilator that can be administered via inhalation. While it is effective in relieving bronchospasm, it is generally used as an adjunct to albuterol and not typically the first-line medication for severe respiratory distress in asthma. Fluticasone is an inhaled corticosteroid that has anti-inflammatory effects and is used for long-term management and control of asthma. It is not appropriate for immediate relief of severe respiratory distress and is not typically used as a first-line medication in the emergency department.
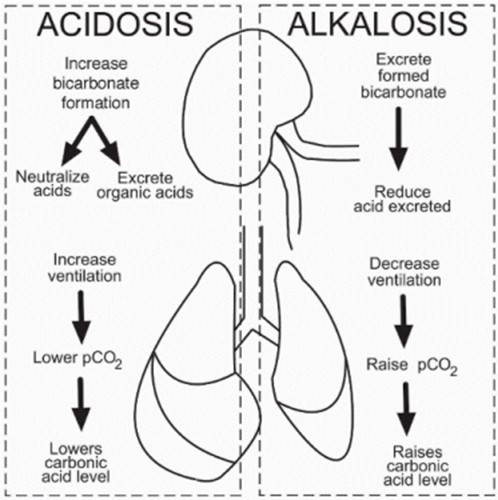
Colleen, a 19 year old Freshman, was drinking alcohol at a frat party. She stupors, falls and hits her head on the ground. Her friend Julie dials "911" because Colleen is now unconscious, depressed ventilation (shallow and slow respirations), rapid heart rate, and is profusely bleeding from both ears. Which primary acid-base imbalance is Colleen at risk for if medical attention is not provided?
Explanation
Respiratory acidosis is a primary acid-base imbalance that occurs when there is an excess of carbon dioxide (CO2) in the body due to impaired ventilation or inadequate removal of CO2 from the lungs. In this case, Colleen's depressed ventilation, indicated by shallow and slow respirations, can lead to inadequate elimination of CO2 from her body. The excessive CO2 levels can result in an accumulation of carbonic acid (H2CO3) in the blood, leading to an increase in acidity and a decrease in pH.
The profuse bleeding from both ears indicates a potential head injury, which can lead to decreased neurological function and impaired control over the respiratory center in the brain. This can further contribute to depressed ventilation and the development of respiratory acidosis. Metabolic acidosis, characterized by a decrease in bicarbonate (HCO3-) levels or an increase in non-carbonic acids in the blood, is not the primary acid-base imbalance in this case since the scenario does not provide information indicating a primary metabolic disorder. Respiratory alkalosis, characterized by decreased levels of CO2 in the blood, leading to increased pH and alkalinity, is not the primary acid-base imbalance in this case. The depressed ventilation and associated increase in CO2 levels indicate the opposite, respiratory acidosis. Metabolic alkalosis, characterized by an increase in bicarbonate levels or a decrease in non-carbonic acids, is not the primary acid-base imbalance in this case as the scenario does not provide information indicating a primary metabolic disorder.
A child diagnosed with Kawasaki disease is brought to the clinic. The mother reports that her child is irritable, refuses to eat, and has skin peeling on both hands and feet. Which intervention should the nurse instruct the mother to implement first?
Explanation
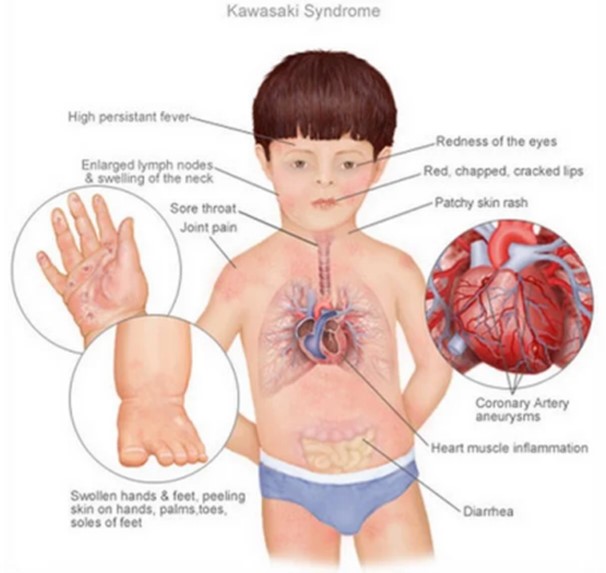
You just viewed 10 questions out of the 44 questions on the RN HESI OB/pediatrics Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



