PN Comprehensive Predictor 2023 (2)
PN Comprehensive Predictor 2023 (2)
Total Questions : 179
Showing 10 questions Sign up for moreThe practical nurse (PN) observes an unlicensed assistive personnel (UAP) performing oral hygiene on an unconscious client who is lying in a flat side-lying position with an emesis basin on the bedside table near the chin. Which action should the PN take?
Explanation
Option A is incorrect because enrolling the UAP in a hospital education class on conducting safe client care does not address the immediate problem or correct the error.
Option B-This would be inappropriate for oral care in an unconscious client as it increases the risk of aspiration.The side-lying position is safer for oral hygiene in unconscious clients.
Option C:While encouraging family participation can be beneficial, it is not the most immediate concern in this situation. The priority is ensuring safe and effective care, which the UAP is providing correctly.
Option D:The flat side-lying position is appropriate for an unconscious client during oral hygiene care. This position helps to prevent aspiration by allowing any secretions or fluids to drain out of the mouth rather than down the throat, which could happen if the client were in a Fowler's position. The presence of the emesis basin near the chin also indicates that the UAP is prepared to catch any fluids, further reducing the risk of aspiration
A woman who delivered a normal newborn 24 hours ago reports, "I seem to be urinating every hour or so. Is that OK?" Which action should the practical nurse (PN) implement?
Explanation
- Urinary output is an important indicator of fluid balance and kidney function. After delivery, a woman may experience increased urinary output due to the loss of excess fluid that was retained during pregnancy and the diuretic effect of oxytocin, which is released during breastfeeding. This is a normal and expected finding in the postpartum period.
- However, increased urinary output may also be a sign of urinary retention, which is the inability to empty the bladder completely. Urinary retention can occur due to trauma to the bladder or urethra during delivery, swelling or hematoma of the perineum, epidural anesthesia, or decreased bladder sensation.Urinary retention can lead to complications such as infection, bladder distension, or postpartum hemorrhage.
- Therefore, when a woman who delivered a normal newborn 24 hours ago reports that she seems to be urinating every hour or so, the practical nurse (PN) should measure the next voiding, then palpate the client's bladder. This will help to assess the amount and quality of urine and the presence or absence of bladder distension. A normal urine output is about 30 ml per hour, and a normal bladder should feel soft and empty after voiding. If the urine output is low or high, or if the bladder feels firm or full after voiding, the PN should report these findings to the primary healthcare provider for further evaluation and intervention.
Therefore, option B is the correct answer, while options A, C, and D are incorrect.
Option A is incorrect because catheterizing the client for residual urine volume is an invasive procedure that should only be done if indicated by the primary healthcare provider.
Option C is incorrect because evaluating for normal involution and massaging the fundus are related to uterine function, not urinary function.
Option D is incorrect because obtaining a specimen for urine culture and sensitivity is not necessary unless there are signs of infection, such as fever, dysuria, or foul-smelling urine.
Prior to giving digoxin, the practical nurse (PN) assesses that a 2-month-old infant's heart rate is 120 beats/minute. Based on this finding, what action should the PN take?
Explanation
a. Administer the medication and alert the charge nurse: This choice suggests proceeding with medication administration but also informing the charge nurse. While it's important to communicate with the charge nurse regarding medication administration, in this scenario, there is no indication to hold the medication as the infant's heart rate is within the normal range. Therefore, alerting the charge nurse may not be necessary at this point.
b. Hold the medication and document cardiac assessment: This choice suggests holding the medication and documenting the cardiac assessment. However, since the infant's heart rate is within the normal range for their age, there is no clinical indication to hold the medication. Holding the medication unnecessarily could delay treatment and potentially lead to adverse outcomes if the medication is needed.
c. Administer the medication and document the heart rate.
Since the infant's heart rate of 120 beats per minute falls within the normal range for a 2-month-old, there is no indication to hold the medication. Administering the digoxin as prescribed and documenting the heart rate before administration are appropriate actions. It's important to ensure accurate documentation to track the infant's response to the medication and monitor for any changes in heart rate.
d. Hold the medication and recheck the heart rate in 1 hour: This choice suggests holding the medication and rechecking the heart rate in 1 hour. Again, since the infant's heart rate is within the normal range, there is no clinical indication to hold the medication or delay treatment. Rechecking the heart rate in 1 hour would be unnecessary and could potentially delay necessary medication administration.
Before administering an antibiotic that can cause nephrotoxicity, which laboratory value is most important for the practical nurse (PN) to review?
Explanation
An antibiotic that can cause nephrotoxicity is an antibiotic that can damage the kidneys, which are the organs that filter the blood and remove waste products and excess fluid from the body. Some examples of nephrotoxic antibiotics are aminoglycosides, vancomycin, amphotericin B, and sulfonamides.
Serum creatinine is a laboratory value that measures the amount of creatinine in the blood. Creatinine is a waste product that is produced by the breakdown of muscle tissue and is normally excreted by the kidneys. A high serum creatinine level indicates that the kidneys are not functioning properly and are unable to filter out the creatinine from the blood.
Before administering an antibiotic that can cause nephrotoxicity, it is important for the practical nurse (PN) to review the serum creatinine level of the client, as it reflects the kidney function and the risk of nephrotoxicity. A normal serum creatinine level ranges from 0.6 to 1.2 mg/dL for men and 0.5 to 1.1 mg/dL for women. If the serum creatinine level is elevated, it may indicate that the client has impaired kidney function or is developing nephrotoxicity from the antibiotic. In this case, the PN should notify the primary healthcare provider and monitor the client for signs and symptoms of nephrotoxicity, such as decreased urine output, edema, hypertension, or electrolyte imbalances .

While receiving report for a client with carcinoma in situ of the left breast, the practical nurse (PN) reviews a pending lab report and notices increased levels of Anti-Glycan Neu5Gc Antibodies (AGNA). Which changes should the PN anticipate to be included in the client's plan of care?
Explanation
- Anti-Glycan Neu5Gc Antibodies (AGNA) are antibodies that recognize a carbohydrate antigen called N- glycolylneuraminic acid (Neu5Gc), which is found in animal-derived foods and tissues, but not in humans. Humans can incorporate Neu5Gc from their diet into their own cells, which can trigger an immune response and the production of AGNA.
- AGNA have been associated with various inflammatory and autoimmune diseases, such as atherosclerosis, rheumatoid arthritis, Crohn's disease, and cancer. AGNA may also play a role in the rejection of bioprosthetic heart valves, which are made from animal tissues that contain Neu5Gc.
- A client with carcinoma in situ of the left breast is a client with a non-invasive form of breast cancer, where the abnormal cells are confined to the ducts or lobules of the breast. This type of cancer has a high chance of cure with surgery and/or radiation therapy.
- Increased levels of AGNA in a client with carcinoma in situ of the left breast may indicate that the client has an increased risk of inflammation and infection, as AGNA can activate the complement system and recruit inflammatory cells to the site of Neu5Gc expression. This may impair the healing process and increase the chances of complications after surgery or radiation therapy.
Therefore, the practical nurse (PN) should anticipate that the client's plan of care will include initiation of changes in infection control measures, such as prophylactic antibiotics, wound care, sterile dressing changes, and monitoring for signs and symptoms of infection (such as fever, redness, swelling, pain, or pus). These measures will help to prevent or treat any potential infection and promote wound healing.
Therefore, option A is the correct answer, while options B, C, and D are incorrect.
Option B is incorrect because increasing the client's dietary servings of fruits and vegetables may not have a significant impact on the levels of AGNA or Neu5Gc in the client's body.
Option C is incorrect because limiting the client's fluid intake to avoid hemodilution may not be necessary or beneficial for the client's condition.
Option D is incorrect because avoiding the client's exposure to cold temperatures may not be relevant or helpful for the client's condition.
At the first dressing change, the practical nurse (PN) tells the client that her mastectomy incision is healing well, but the client refuses to look at the incision and refuses to talk about it. Which response by the PN to the client's silence is best?
Explanation
- A mastectomy is a surgical procedure that involves the removal of all or part of the breast, usually to treat breast cancer. A mastectomy can have a significant impact on a woman's physical, emotional, and psychological well-being, as it may affect her body image, self-esteem, sexuality, and identity.
- A mastectomy incision is the wound that results from the surgery, which may vary in size, shape, and location depending on the type and extent of the mastectomy. The incision may be closed with stitches, staples, or glue, and covered with a dressing or bandage.
- The first dressing change is usually done within 24 to 48 hours after the surgery, and it involves removing the old dressing, inspecting the incision for any signs of infection or complications, cleaning the wound, applying a new dressing, and educating the client about wound care .
- When the practical nurse (PN) tells the client that her mastectomy incision is healing well, but the client refuses to look at the incision and refuses to talk about it, this may indicate that the client is experiencing denial, fear, anger, grief, or depression due to the loss of her breast. These are normal and common reactions that may occur at different stages of the recovery process .
- The best response by the PN to the client's silence is to acknowledge and respect the client's feelings, provide support and reassurance, and offer assistance when needed. This will help to establish trust and rapport with the client, as well as promote her coping and adjustment .
- Therefore, option A is the best answer, as it shows empathy and respect for the client's feelings, while also informing the client that the PN will be available when she is ready to look or talk about the mastectomy. Option A also implies that the PN will not pressure or force the client to do something that she is not comfortable with.
- Options B, C, and D are incorrect answers, as they do not show empathy or respect for the client's
feelings, and they may cause more harm than good.
Option B is incorrect because asking another nurse to be present may not address the client's reluctance or
anxiety about looking at her incision.
Option C is incorrect because telling the client that part of recovery is accepting her new body image may
sound insensitive or judgmental, and it may not reflect the client's readiness or willingness to do so.
Option D is incorrect because telling the client that she will feel beter when she sees that the incision is not as bad as she may think may minimize or invalidate the client's feelings, and it may not be true or helpful.
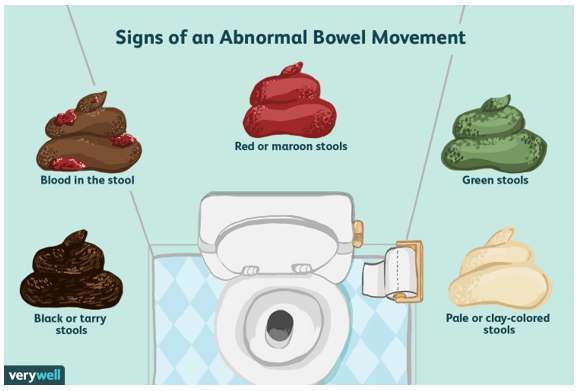
When performing a focused gastrointestinal system assessment, the practical nurse (PN) asks a male client when his last bowel movement occurred. The client answers, "Three days ago."
Which action should the PN implement first?
Explanation
A bowel patern is the frequency, consistency, and appearance of a person's bowel movements. A normal bowel patern is what's normal for each person, and it can vary depending on factors such as diet, age, physical activity, and health conditions.
A focused gastrointestinal system assessment includes collecting subjective data about the patient's history of gastrointestinal disease, signs and symptoms of gastrointestinal problems, diet and nutrition, and bowel patern. It also includes inspecting and auscultating the abdomen for any abnormalities.
When a client reports having a bowel movement three days ago, the first action that the practical nurse should implement is to determine the client's usual bowel patern. This will help to evaluate if the client is experiencing constipation or if this is their normal frequency. It will also help to identify any changes or risk factors that may affect the client's bowel function.
The practical nurse (PN) is caring for a client whose urine drug screen is positive for cocaine. Which behavior is most likely seen in this client?
Explanation
- Cocaine is a powerfully addictive stimulant drug that increases the levels of dopamine in the brain, which is a chemical messenger related to movement, pleasure, and motivation.
- Cocaine's effects appear almost immediately and last for a few minutes to an hour, depending on the method of use. Some of the short-term effects of cocaine include extreme happiness and energy, mental alertness, hypersensitivity to sight, sound, and touch, and irritability.
- An elevated energy level is one of the most common and noticeable effects of cocaine use, as cocaine stimulates the central nervous system and makes the user feel more alert, active, and confident¹². This effect may also lead to increased physical activity, talkativeness, or aggression.
Therefore, option A is the correct answer, while options B, C, and D are incorrect.
Option B is incorrect because a powerful craving for more cocaine is not a behavior that can be observed by others, but rather an internal feeling that the user may experience due to the addictive nature of the drug.
Option C is incorrect because high self-esteem is not a typical effect of cocaine use, as cocaine may cause paranoia or anxiety in some users.
Option D is incorrect because euphoria is not a behavior that can be observed by others, but rather an emotional state that the user may feel due to the increased dopamine levels in the brain

The practical nurse (PN) observes a newly hired unlicensed assistive personnel (UAP) who is counting a client's radial pulse as seen in the picture.
Which action should the PN take?

Explanation
A radial pulse is the pulse felt at the wrist, where the radial artery runs along the thumb side of the forearm. It is one of the most common sites for measuring a person's heart rate⁴.
To measure a radial pulse, the examiner should place two or three fingers over the radial artery, just below the wrist crease, and apply gentle pressure until a pulsation is felt. The examiner should not use the thumb, as it has its own pulse and may interfere with the accuracy of the measurement. The examiner should count the number of beats for 15, 30, or 60 seconds, depending on the regularity and rate of the pulse³⁵.
In the picture, the unlicensed assistive personnel (UAP) is using the thumb to measure the radial pulse, which is incorrect. The practical nurse (PN) should demonstrate the correct pulse site to the UAP and explain why using the thumb is not appropriate. This will help to ensure that the UAP obtains an accurate and reliable pulse rate for the client.
The practical nurse (PN) is told that she keeps her 2-year-old child in a playpen so he will not get dirty. Which statement should the PN use in responding to this concern about using a playpen?
Explanation
- A playpen is a portable enclosure that provides a confined space for a child to play in. It can be useful for keeping a child safe and supervised when the caregiver is busy or needs a break, but it should not be used as a substitute for active play or interaction with the caregiver or others.
- A 2-year-old child is in the developmental stage of toddlerhood, which is characterized by rapid physical, cognitive, social, and emotional growth. Toddlers are curious and eager to learn about the world around them, and they need opportunities to explore, experiment, and manipulate objects and materials. They also need stimulation, guidance, and feedback from their caregivers and peers to develop their language, problem-solving, and social skills.
- Keeping a 2-year-old child in a playpen for long periods of time or to prevent them from getting dirty can have negative effects on their development and well-being. It can limit their physical activity, creativity, and independence, and it can cause boredom, frustration, or resentment . It can also interfere with their atachment and bonding with their caregiver, as well as their self-esteem and self-image.
- Therefore, the practical nurse (PN) should use the statement "Children need time to actively explore their environment" in responding to this concern about using a playpen. This statement reflects the developmental needs and rights of the child, and it encourages the caregiver to provide a more stimulating and supportive environment for the child. It also implies that getting dirty is not a problem, but rather a natural and healthy part of play and learning.
- Therefore, option D is the correct answer, while options A, B, and C are incorrect. Option A is incorrect because it is judgmental and may offend or discourage the caregiver.
Option B is incorrect because it is not true that playpens provide a sense of security for the child, as they may feel isolated or restricted in them.
Option C is incorrect because it is not true that playpens provide a safe environment for a toddler, as they may pose hazards such as entrapment, suffocation, or injury from falling or climbing out of them.

You just viewed 10 questions out of the 179 questions on the PN Comprehensive Predictor 2023 (2) Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



