Before administering an antibiotic that can cause nephrotoxicity, which laboratory value is most important for the practical nurse (PN) to review?
Serum calcium
Serum creatinine
Hemoglobin and Hematocrit
White blood cell count (WBC)
The Correct Answer is B
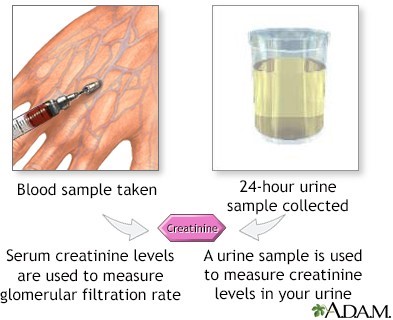
Serum creatinine is the most important laboratory value to review before administering an antibiotic that can cause nephrotoxicity. Nephrotoxicity is an alteration in the function of the kidney due to exposure to certain drugs or toxins.
It can be assessed by measuring the glomerular filtration rate (GFR), which is the rate of clearance of a substance from the blood by the kidneys. Serum creatinine is a waste product of muscle metabolism that is freely filtered by the glomeruli and not reabsorbed or secreted by the tubules.
Therefore, it is a reliable indicator of GFR and renal function. An increase in serum creatinine indicates a decrease in GFR and renal function, which may be caused by nephrotoxic drugs.
The other laboratory values are not directly related to nephrotoxicity or GFR:
- Serum calcium: This may be affected by renal function, but it is not a sensitive or specific marker of nephrotoxicity. It may be altered by other factors such as vitamin D, parathyroid hormone, and bone metabolism.
- Hemoglobin and hematocrit: These may be affected by renal function, but they are not sensitive or specific markers of nephrotoxicity. They may reflect the erythropoietin production by the kidneys, which stimulates red blood cell production in the bone marrow. However, they may also be influenced by other factors such as blood loss, hydration status, and iron deficiency.
- White blood cell count (WBC): This is not related to nephrotoxicity or GFR. It may reflect the presence of infection or inflammation, which may be a cause or a consequence of renal impairment, but it is not a direct measure of renal function.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
The correct answer is B. "You seem quite frightened right now."
Choice A rationale:
This statement dismisses the client's feelings and may not provide the reassurance they need. It could also escalate the situation if the client feels misunderstood or ignored.
Choice B rationale:
This response acknowledges the client's emotions and validates their experience, which can help build trust and de-escalate the situation. It shows empathy and understanding, which are crucial in managing delusions.
Choice C rationale:
While this statement aims to reassure the client, it may not address their immediate emotional state. The client might not feel safe despite being told they are, so it might not be as effective in calming them down.
Choice D rationale:
This response could inadvertently reinforce the client's delusions by implying that their fears are valid and that the nurse should take action based on those delusions. It might also confuse the client further.
Correct Answer is ["C","E"]
Explanation
Choice A rationale:
A bedside commode is positioned near the bed. Positioning a bedside commode near the bed is appropriate for a client with heart failure and COPD who may have mobility issues or difficulty walking to the bathroom. It promotes safety and convenience for the client.
Choice B rationale:
A full pitcher of water is on the bedside table. While it's essential to keep clients with heart failure adequately hydrated, having a full pitcher of water within easy reach might encourage excessive fluid intake, which can exacerbate heart failure symptoms. However, this choice is not an immediate risk requiring intervention.
Choice C rationale:
The client is lying in a supine position in bed. A client with heart failure and COPD should not be lying in a supine position because it can exacerbate respiratory distress and increase the workload of the heart. This is an observation that requires immediate intervention, such as repositioning the client to an upright or semi-fowler's position.
Choice D rationale:
A saline lock is present in the right forearm. The presence of a saline lock is a standard precaution in a hospitalized client and does not require immediate intervention unless there are specific issues with it, such as signs of infection or dislodgement. It does not pose an immediate harm to the client.
Choice E rationale:
A low sodium diet tray was brought to the room. A low sodium diet is crucial for managing heart failure because excessive sodium intake can lead to fluid retention and exacerbate symptoms. Ensuring that the client follows the prescribed diet is essential for their well-being, and any deviations may require immediate intervention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
