LPN Med Surg neuro test 2024
ATI LPN Med Surg neuro test 2024
Total Questions : 44
Showing 10 questions Sign up for moreA nurse is caring for a client in the emergency department who has a preliminary diagnosis of a transient ischemic attack (TIA). Which of the following diagnostic testing should the nurse anticipate the provider to prescribe?
Explanation
A.Computerized tomography angiography (CTA)
This is a likely diagnostic test that the provider may prescribe. CTA uses computed tomography (CT) imaging to visualize the blood vessels in the brain and neck. It can help identify areas of stenosis, occlusion, or other abnormalities in the blood vessels that may contribute to the TIA symptoms.
B. Complete blood count (CBC)
A complete blood count (CBC) is a routine laboratory test that assesses various components of blood, such as red blood cells, white blood cells, and platelets. While it may not be specific to diagnosing a transient ischemic attack (TIA), it can help evaluate for underlying conditions such as anemia or thrombocytosis that could contribute to TIA symptoms or increase the risk of stroke.
C. Prothrombin time (PT)
Prothrombin time (PT) is a laboratory test that evaluates the clotting ability of blood and is typically used to monitor anticoagulant therapy. While abnormal coagulation parameters may be associated with certain conditions that predispose to TIA (such as atrial fibrillation), PT alone is not a specific diagnostic test for TIA.
D. Transesophageal echocardiogram (TEE)
This is another possible diagnostic test that the provider may prescribe. TEE is a specialized echocardiogram that provides detailed images of the heart structures by inserting an ultrasound probe
A nurse is reinforcing discharge teaching to a client who has epilepsy. Which of the following instructions should be included in the teaching?
Explanation
A. Placing padding around or under the patient's head
This is a helpful instruction to include. Placing padding around or under the patient's head can help prevent injury during a seizure by cushioning the head against impact with the ground.
B. Positioning the patient on the side once the relaxation stage is entered to allow oral secretions to drain
This is a correct instruction. Positioning the patient on their side (recovery position) can help prevent aspiration if vomiting occurs during or after the seizure. It also helps clear oral secretions and maintain a clear airway.
C. Having the necessary equipment and/or personnel in case the patient doesn't spontaneously breathe when the seizure is over
This is an important instruction. It is crucial to have emergency equipment (such as oxygen and suction) readily available and to be prepared to provide respiratory support if the patient does not spontaneously breathe after the seizure.
D. Inserting a tongue depressor in the patient's mouth
This is an incorrect instruction. It is not recommended to insert anything into the patient's mouth during a seizure as it can cause injury to the teeth, gums, or airway. Additionally, it is a common misconception that tongue swallowing occurs during seizures, which is rare.
E. Noting the time the seizure started
This is a critical instruction. Noting the time the seizure started helps healthcare providers assess the duration of the seizure and determine if medical intervention is necessary. It also helps monitor the patient's recovery and response to treatment.
F. Holding the patient down to prevent injury
This is an incorrect instruction. Holding the patient down during a seizure can cause injury to both the patient and the person restraining them. It is important to create a safe environment by removing hazards and guiding the patient away from dangerous objects or situations, but holding them down is not appropriate.
A nurse is providing discharge instruction to a client who has hypertension that has resulted in a transient ischemic attack (TIA). Which of the following information should the nurse discuss with the client regarding blood pressure (BP) management?
Explanation
A. The client should maintain systolic BP between 120 and 129 mm Hg.
This is an appropriate recommendation. The American Heart Association (AHA) guidelines recommend maintaining systolic BP below 130 mm Hg to reduce the risk of stroke and other cardiovascular events in individuals with a history of stroke or TIA.
B. The client should maintain systolic BP between 130 and 135 mm Hg.
This is slightly above the recommended range. While systolic BP below 135 mm Hg is generally recommended for individuals with a history of stroke or TIA, a range of 130-135 mm Hg may still be acceptable based on individual patient factors and risk assessments.
C. The client should maintain systolic BP between 136 and 140 mm Hg.
This is above the recommended range. Systolic BP between 136 and 140 mm Hg may be considered elevated and should be managed to lower levels to reduce the risk of recurrent TIA or stroke.
D. The client should maintain systolic BP between 141 and 145 mm Hg.
This is above the recommended range. Systolic BP above 140 mm Hg is generally considered elevated and should be managed to lower levels to reduce the risk of recurrent TIA or stroke.
Which signs and symptoms characterize expressive aphasia?
Explanation
A. Difficulty initiating speech
This is a characteristic symptom of expressive aphasia. Individuals with expressive aphasia have difficulty initiating speech and may produce speech that is slow, effortful, and lacking in grammatical structure.
B. Difficulty understanding the written and spoken word
This symptom is not typically associated with expressive aphasia. Instead, difficulty understanding language, both written and spoken, is more commonly seen in receptive aphasia, also known as Wernicke's aphasia.
C. Total inability to communicate
While expressive aphasia can severely impair verbal communication, it does not result in a total inability to communicate. Individuals with expressive aphasia may still be able to communicate to some extent using nonverbal means, gestures, or writing.
D. Stuttering and spitting
Stuttering and spitting are not characteristic symptoms of expressive aphasia. Stuttering is a speech disorder characterized by interruptions in the flow of speech, while spitting is not typically associated with aphasia.
On admission to the emergency department, a patient with a C5 compression fracture can move only his head and has flaccid paralysis of all extremities. The distraught family asks if the paralysis is permanent. Which is the best response by the nurse?
Explanation
A. "It is too early to tell. When the spinal shock subsides, we will know more."
This response is appropriate. Spinal shock can initially obscure the extent of neurological injury, and it may take time for the full extent of the injury to become apparent. By acknowledging this and suggesting that more information will be available once spinal shock subsides, the nurse provides a realistic perspective without prematurely predicting the outcome.
B. "You should talk to your physician about things of that nature."
This response may come across as dismissive or evasive. While it is true that the physician ultimately determines the patient's prognosis, the family may be seeking reassurance and guidance from the nurse as well.
C. "No. Significant recovery of function should occur in a few days."
This response is overly optimistic and potentially misleading. While some improvement may occur in the days following a spinal cord injury, significant recovery of function within a few days is unlikely, especially in cases of flaccid paralysis of all extremities.
D. "Yes. In all likelihood, the paralysis is probably permanent."
This response is overly pessimistic and lacks sensitivity. It may unnecessarily distress the family and extinguish hope for the patient's recovery.
Which neurologic finding would be considered abnormal in an 88-year-old patient?
Explanation
A. Dizziness and problems with balance
While dizziness and problems with balance can occur more frequently in older adults due to age-related changes in the vestibular system and other factors, persistent or severe dizziness or balance issues should be evaluated further as they could indicate underlying neurological or medical conditions.
B. Slow papillary response to light
This finding may be considered abnormal, especially if it represents a significant change from the individual's baseline. While age-related changes in pupil function can occur, a slow or sluggish pupillary response to light may indicate dysfunction of the oculomotor nerve or other neurological issues and should be investigated further.
C. Jerky eye movements
Jerky eye movements, such as nystagmus, can be abnormal and may indicate dysfunction of the vestibular system or other neurological conditions. While some degree of nystagmus can occur with age, persistent or severe jerky eye movements should be evaluated further.
D. Absence of the Achilles tendon jerk
This finding may also be considered abnormal. The Achilles tendon reflex, tested using the deep tendon reflex (DTR) examination, can diminish with age but should not be completely absent in the absence of specific medical conditions affecting the reflex arc or spinal cord function.
Which position should a nurse instruct a patient to assume after a lumbar puncture to prevent a headache?
Explanation
A. Lie flat:
This option involves instructing the patient to lie flat on their back without elevating their head. Lying flat helps to maintain consistent pressure in the spinal canal, reducing the likelihood of CSF leakage from the puncture site. This position is commonly recommended after a lumbar puncture to prevent or minimize the occurrence of post-lumbar puncture headaches (PLPH).
B. Lie on left side:
This option involves instructing the patient to lie on their left side. While lying on the left side may provide some relief by reducing pressure on the lumbar puncture site, it is not typically recommended immediately after the procedure to prevent PLPH. Lying flat is generally preferred to minimize changes in CSF pressure and reduce the risk of headache.
C. Stay in semi-Fowler position:
The semi-Fowler position involves elevating the head of the bed at a 30-45 degree angle. This position is not typically recommended immediately after a lumbar puncture because it may increase CSF leakage and pressure changes, potentially exacerbating the risk of developing a headache.
D. Ambulate in the room with assistance:
Ambulating shortly after a lumbar puncture is not typically recommended as it may increase the risk of developing a headache. Movement and changes in posture can exacerbate CSF leakage and pressure changes at the puncture site, leading to the development of post-lumbar puncture headaches.
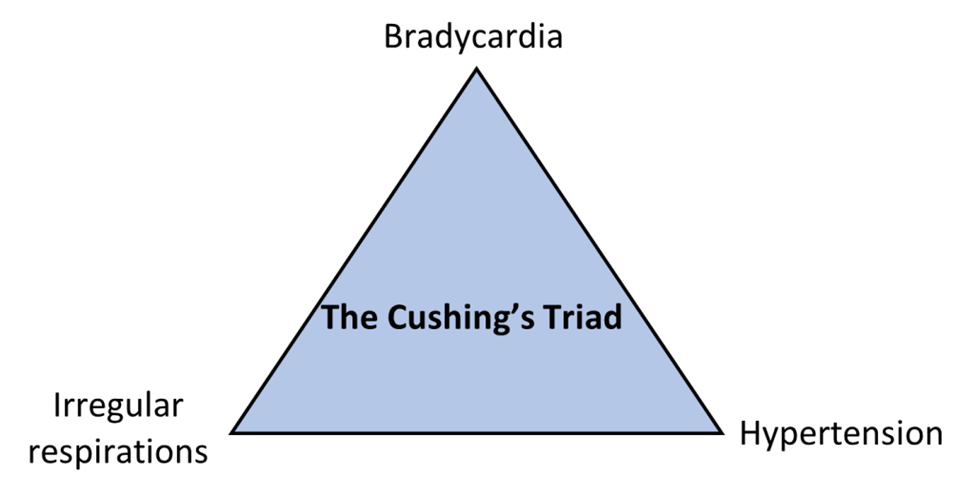
Which three symptoms are characteristic of Cushing triad associated with increased ICP?
Explanation
A. Bradycardia, hypertension, and widening pulse pressure
This combination of symptoms is characteristic of Cushing's triad. Bradycardia (slow heart rate), hypertension (elevated blood pressure), and widening pulse pressure (difference between systolic and diastolic blood pressure) are indicative of increased ICP, specifically resulting in the compression of brain structures that regulate vital functions.
B. Widening pulse pressure, headache, and seizure
While headache and seizure may occur in patients with increased ICP, widening pulse pressure alone is not sufficient to meet the criteria of Cushing's triad. The presence of bradycardia and hypertension, along with widening pulse pressure, is more indicative of Cushing's triad.
C. Hypertension, tachycardia, and headache
Hypertension and headache may occur in patients with increased ICP, but the absence of bradycardia and widening pulse pressure makes this option less characteristic of Cushing's triad.
D. Hypotension, tachycardia, and narrowing pulse pressure
Hypotension (low blood pressure) and narrowing pulse pressure are not typically associated with Cushing's triad. Tachycardia (rapid heart rate) may occur in response to increased ICP, but it is usually accompanied by bradycardia rather than hypotension.
A patient is stuporous but reacts by withdrawing from painful stimuli. Which term is most appropriate for this patient?
Explanation
A. Semicomatose:
This term suggests a state between consciousness and coma. A patient who is semicomatose may exhibit some level of responsiveness but is typically unresponsive or only responds to intense stimuli.
B. Somnolent:
Somnolence refers to a state of drowsiness or sleepiness. A somnolent patient may appear sleepy, have difficulty staying awake, and may be slow to respond to stimuli. However, the withdrawal from painful stimuli described in the scenario suggests a higher level of responsiveness than what would typically be expected in a somnolent state.
C. Lethargic:
Lethargy describes a state of reduced alertness or responsiveness. A lethargic patient may appear drowsy, sluggish, and have diminished responses to stimuli. The description of the patient as stuporous (having a decreased level of consciousness) but still reacting by withdrawing from painful stimuli aligns with the characteristics of lethargy.
D. Comatose:
Coma refers to a state of profound unconsciousness where the patient is unresponsive to all stimuli, including painful stimuli. A comatose patient does not demonstrate any purposeful movement or response to stimuli. Since the patient in the scenario exhibits some response to painful stimuli by withdrawing, they do not meet the criteria for being comatose.
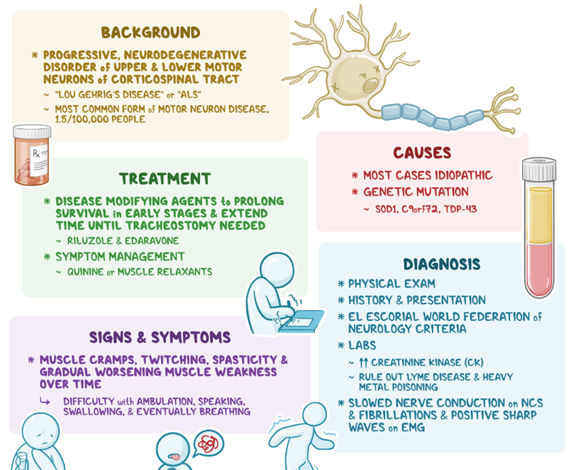
Which reason explains why a patient with amyotrophic lateral sclerosis (ALS) is uniquely prone to depression?
Explanation
A. Intellectual capacity is not affected:
This statement refers to the fact that ALS primarily affects motor neurons, leading to muscle weakness and paralysis, but it typically does not directly impact cognitive function or intellectual capacity. While cognitive impairment is not a hallmark feature of ALS, some individuals may experience changes in cognitive function or behavior, such as executive dysfunction or frontotemporal dementia, in later stages of the disease. However, depression in ALS is not primarily linked to changes in intellectual capacity but rather to other factors such as altered communication, physical limitations, and loss of autonomy.
B. Communication is altered:
ALS can affect the muscles involved in speech and swallowing, leading to difficulties in communicationAs the disease progresses, patients may experience dysarthria (difficulty speaking clearly) and dysphagia (difficulty swallowing), which can impair their ability to communicate effectively with others. Altered communication can result in frustration, social isolation, and feelings of being misunderstood, all of which are risk factors for depression.
C. Mobility is limited:
ALS causes progressive muscle weakness and paralysis, which can significantly impair mobility over time. As the disease advances, individuals with ALS may become increasingly dependent on mobility aids such as wheelchairs or may require assistance with mobility tasks. Limited mobility can lead to feelings of loss of independence, decreased participation in activities, and increased dependence on caregivers, all of which can contribute to depression.
D. Nutritional intake is poor:
ALS can affect the muscles involved in swallowing and chewing, leading to difficulties with eating and drinking. Dysphagia, or difficulty swallowing, is a common symptom in ALS and can result in poor nutritional intake and weight loss. Malnutrition and weight loss are associated with increased morbidity and mortality in ALS, and they can also contribute to feelings of weakness, fatigue, and overall decline in quality of life, which may exacerbate depression.
You just viewed 10 questions out of the 44 questions on the ATI LPN Med Surg neuro test 2024 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



