On admission to the emergency department, a patient with a C5 compression fracture can move only his head and has flaccid paralysis of all extremities. The distraught family asks if the paralysis is permanent. Which is the best response by the nurse?
"It is too early to tell. When the spinal shock subsides, we will know more."
"You should talk to your physician about things of that nature."
"No. Significant recovery of function should occur in a few days."
"Yes. In all likelihood, the paralysis is probably permanent."
The Correct Answer is A
A. "It is too early to tell. When the spinal shock subsides, we will know more."
This response is appropriate. Spinal shock can initially obscure the extent of neurological injury, and it may take time for the full extent of the injury to become apparent. By acknowledging this and suggesting that more information will be available once spinal shock subsides, the nurse provides a realistic perspective without prematurely predicting the outcome.
B. "You should talk to your physician about things of that nature."
This response may come across as dismissive or evasive. While it is true that the physician ultimately determines the patient's prognosis, the family may be seeking reassurance and guidance from the nurse as well.
C. "No. Significant recovery of function should occur in a few days."
This response is overly optimistic and potentially misleading. While some improvement may occur in the days following a spinal cord injury, significant recovery of function within a few days is unlikely, especially in cases of flaccid paralysis of all extremities.
D. "Yes. In all likelihood, the paralysis is probably permanent."
This response is overly pessimistic and lacks sensitivity. It may unnecessarily distress the family and extinguish hope for the patient's recovery.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
A. Aura phase:
The aura phase occurs before the seizure and is characterized by subjective sensations or experiences that some individuals may have. It serves as a warning sign that a seizure is about to occur. This phase precedes the seizure itself and is not applicable to the period immediately afterward.
B. Presence of automatisms:
Automatisms refer to repetitive, involuntary movements or actions that some individuals may exhibit during certain types of seizures, such as complex partial seizures. They are not typically observed during the postictal phase of a generalized tonic-clonic seizure.
C. Postictal phase:
The postictal phase, also known as the postictal state, refers to the period following a seizure during which the individual may experience confusion, drowsiness, or other altered states of consciousness. This phase typically lasts for minutes to hours and is characterized by gradual recovery of normal function.
D. Presence of absence seizures:
Absence seizures are characterized by brief episodes of altered consciousness, often manifesting as staring spells or momentary loss of awareness. They are distinct from generalized tonic-clonic seizures and do not involve the same postictal phase characterized by drowsiness and altered arousal.
Correct Answer is C
Explanation
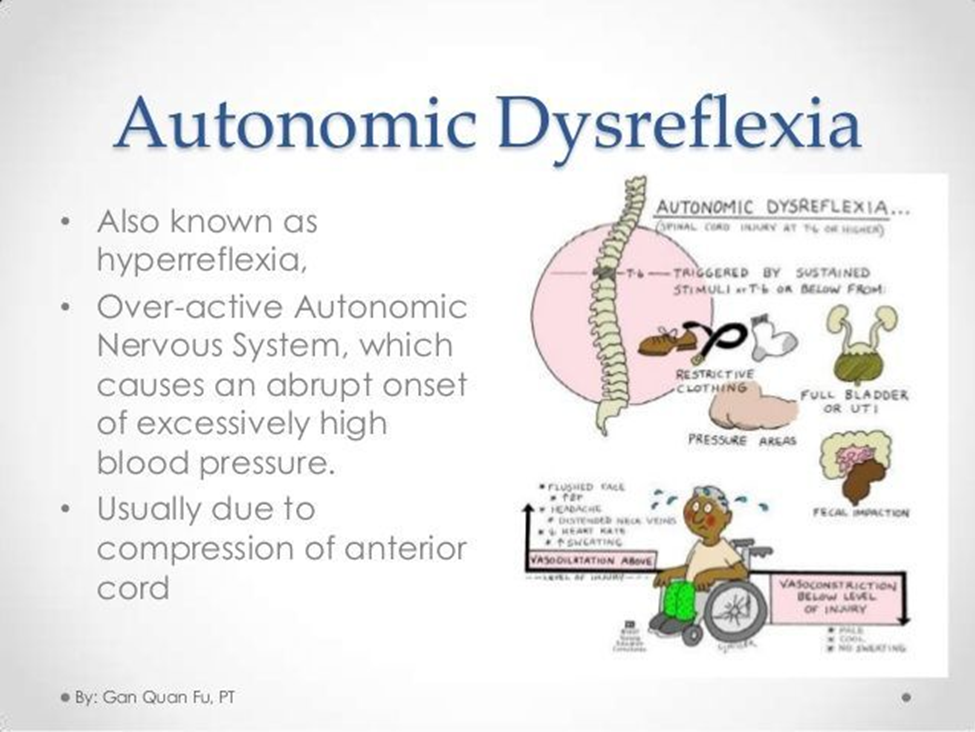
A. Check the client for a fecal impaction.
This intervention is important for managing autonomic dysreflexia because a fecal impaction can trigger autonomic dysreflexia by causing rectal distention. However, it is not the first action the nurse should take. Promptly addressing the immediate cause of autonomic dysreflexia is crucial to prevent complications.
B. Ensure the room temperature is warm.
This intervention is important for maintaining the client's comfort and preventing temperature-related complications. However, it is not the first action the nurse should take when suspecting autonomic dysreflexia. Immediate interventions to address the underlying cause of autonomic dysreflexia are necessary to prevent serious complications such as stroke or seizure.
C. Check the client's bladder for distention.
This is the correct action to take first. Bladder distention is one of the most common triggers of autonomic dysreflexia in individuals with spinal cord injuries. A distended bladder stimulates autonomic reflexes, leading to a sudden increase in blood pressure. Therefore, the nurse should assess the client's bladder for distention and initiate appropriate interventions such as catheterization to relieve urinary retention.
D. Raise the head of the bed.
While elevating the head of the bed can help reduce blood pressure in some situations, it is not the first action the nurse should take when suspecting autonomic dysreflexia. Elevating the head of the bed may exacerbate autonomic dysreflexia by increasing venous return and blood pressure. Therefore, addressing the underlying cause of autonomic dysreflexia, such as bladder distention, takes priority.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
