PN Adult Medical Surgical 2020 with NGN
ATI PN Adult Medical Surgical 2020 with NGN
Total Questions : 78
Showing 10 questions Sign up for moreA nurse is caring for a client who is at risk for anaphylaxis due to bee stings. When reinforcing teaching about the use of an automatic epinephrine injector, which of the following actions is the priority?
Explanation
Choice A: Instructing the client to store the injector at room temperature is not the priority because it is not a life-saving action. Storing the injector at room temperature is important to maintain its effectiveness and prevent damage from heat or cold. However, it is not as urgent as seeking medical attention or recognizing anaphylaxis.
Choice B: Informing the client to seek medical attention following administration of the injection is the priority because it is a life-saving action. Seeking medical attention following administration of the injection is essential to prevent further complications or recurrence of anaphylaxis. Anaphylaxis is a severe allergic reaction that can cause symptoms such as difficulty breathing, swelling, rash, or shock. It can be fatal if not treated promptly and properly. Epinephrine is a medication that can reverse some of the symptoms of anaphylaxis by constricting blood vessels, relaxing airways, and increasing heart rate. However, epinephrine is not a cure for anaphylaxis and its effects may wear off after 15 to 20 minutes. Therefore, the client should seek medical attention as soon as possible after using the injector.
Choice C: Having the client perform a return demonstration of the equipment is not the priority because it is not a life-saving action. Having the client perform a return demonstration of the equipment is important to assess the client's understanding and ability to use the injector correctly. However, it is not as urgent as seeking medical attention or recognizing anaphylaxis.
Choice D: Reviewing the signs of anaphylaxis with the client is not the priority because it is not a life-saving action. Reviewing the signs of anaphylaxis with the client is important to educate the client about how to identify and respond to an allergic reaction. However, it is not as urgent as seeking medical attention or using the injector.
A nurse is assisting in the care of a client who has a pulmonary embolism and is experiencing dyspnea. Which of the following actions should the nurse take first?
Explanation
Choice A reason: Administering heparin to the client is an important intervention, but it is not the first action the nurse should take. Heparin is an anticoagulant that prevents further clot formation, but it does not dissolve existing clots or improve oxygenation.
Choice B reason: Encouraging the client to cough and deep breathe is a helpful measure to promote lung expansion and expectoration of secretions, but it is not the first action the nurse should take. Coughing and deep breathing may also increase the client's dyspnea and anxiety.
Choice C reason: Obtaining the client's vital signs is a necessary step to monitor the client's condition, but it is not the first action the nurse should take. Vital signs may indicate hypoxia, tachycardia, hypotension, or other signs of shock, but they do not address the immediate problem of impaired gas exchange.
Choice D reason: Placing the client in high-Fowler's position is the first action the nurse should take. This position allows for maximum lung expansion and improves oxygenation. It also reduces venous return and cardiac workload, which may decrease pulmonary artery pressure and right ventricular strain.
A nurse is caring for a client who has pneumonia with dyspnea. The client's ABG results are pH 7.30, PaCO2 50 mm Hg, HCO3 26 mEq/L. The nurse should recognize that the client has which of the following acid-base imbalances?
Explanation
Choice A reason: Metabolic alkalosis is a condition in which the pH is high and the HCO3 is high. This can be caused by excessive vomiting, diuretic use, or ingestion of antacids. The client's ABG results do not indicate metabolic alkalosis.
Choice B reason: Respiratory alkalosis is a condition in which the pH is high and the PaCO2 is low. This can be caused by hyperventilation, anxiety, or fever. The client's ABG results do not indicate respiratory alkalosis.
Choice C reason: Metabolic acidosis is a condition in which the pH is low and the HCO3 is low. This can be caused by diabetic ketoacidosis, renal failure, or diarrhea. The client's ABG results do not indicate metabolic acidosis.
Choice D reason: Respiratory acidosis is a condition in which the pH is low and the PaCO2 is high. This can be caused by hypoventilation, airway obstruction, or lung disease. The client's ABG results indicate respiratory acidosis, which means that the client has impaired gas exchange and retention of carbon dioxide.
A nurse is reviewing laboratory values of a client who has severe dyspnea. Which of the following laboratory values indicates heart failure?
Explanation
Choice A reason: Potassium 4.0 mEq/L is a normal value for serum potassium. Potassium is an electrolyte that regulates nerve and muscle function, cardiac rhythm, and fluid balance. Abnormal levels of potassium can indicate renal dysfunction, dehydration, or acid-base imbalance, but not heart failure.
Choice B reason: Calcium 9.0 mg/dL is a normal value for serum calcium. Calcium is an electrolyte that regulates bone health, muscle contraction, blood clotting, and nerve transmission. Abnormal levels of calcium can indicate parathyroid dysfunction, vitamin D deficiency, or malignancy, but not heart failure.
Choice C reason: Sodium 140 mEq/L is a normal value for serum sodium. Sodium is an electrolyte that regulates fluid balance, blood pressure, and nerve and muscle function. Abnormal levels of sodium can indicate dehydration, fluid overload, or hormonal imbalance, but not heart failure.
Choice D reason: Brain natriuretic peptide (BNP) 275 pg/mL is an elevated value for serum BNP. BNP is a hormone that is released by the heart when it is stretched or stressed due to increased pressure or volume overload. BNP causes diuresis, vasodilation, and decreased blood pressure to reduce the workload of the heart. Elevated levels of BNP indicate heart failure, which means that the heart cannot pump enough blood to meet the body's needs.
A nurse is contributing to the plan of care for a client who has heart failure. Which of the following actions should the nurse include in the plan?
Explanation
Choice A rationale:
Encouraging fluids is not appropriate for a client with heart failure. Clients with heart failure often experience fluid overload due to the heart’s inability to pump effectively, leading to fluid retention.Encouraging additional fluid intake can exacerbate this condition, worsening symptoms such as edema and shortness of breath.
Choice B rationale:
Measuring vital signs every 8 hours may not be frequent enough for a client with heart failure, especially if they are experiencing acute symptoms.More frequent monitoring is often necessary to detect changes in the client’s condition promptly and to manage symptoms effectively.
Choice C rationale:
Obtaining weight weekly is not sufficient for a client with heart failure. Daily weight monitoring is crucial as it helps in detecting fluid retention early.Sudden weight gain can indicate worsening heart failure and the need for adjustments in treatment.
Choice D rationale:
Allowing frequent rest periods is essential for clients with heart failure. These clients often experience fatigue and decreased exercise tolerance due to reduced cardiac output.Frequent rest periods help in managing fatigue and preventing overexertion, which can worsen heart failure symptoms.
A nurse is performing tracheostomy care for a client who has a chronic tracheostomy. Which of the following actions should the nurse take?
Explanation
Choice A reason: Allowing space for one finger to be placed under the tube ties is a correct action for tracheostomy care. This ensures that the tube ties are not too tight, which can cause skin breakdown, pressure necrosis, or impaired circulation. The tube ties should also not be too loose, which can cause accidental dislodgement of the tube.
Choice B reason: Applying suction pressure while inserting the catheter into the trachea is an incorrect action for tracheostomy care. This can cause trauma to the tracheal mucosa and increase the risk of infection and bleeding. The nurse should apply suction pressure only while withdrawing the catheter and rotate it gently to remove secretions.
Choice C reason: Suctioning the client for 20 seconds with each pass is an incorrect action for tracheostomy care. This can cause hypoxia, bradycardia, or cardiac arrest due to vagal stimulation. The nurse should suction the client for no more than 10 to 15 seconds with each pass and allow at least 30 seconds between passes for oxygenation.
Choice D reason: Cleansing around the stoma with povidone-iodine is an incorrect action for tracheostomy care. Povidone-iodine is a strong antiseptic that can irritate the skin and cause allergic reactions. The nurse should cleanse around the stoma with normal saline or sterile water and apply a thin layer of water-soluble lubricant to protect the skin.
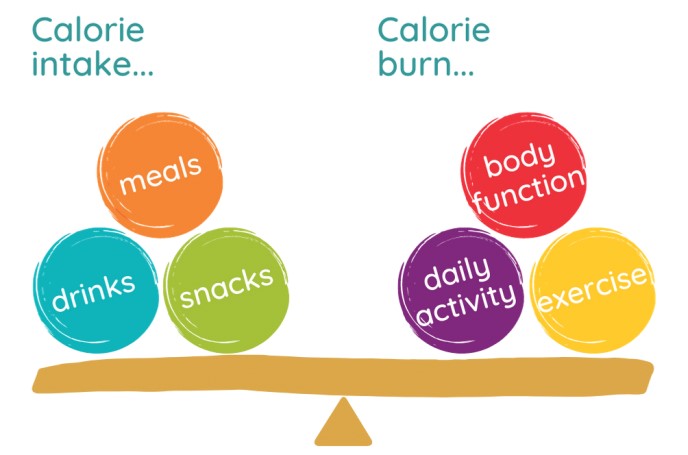
A nurse is reinforcing teaching with a client who wants to lose 0.9 kg (2 lb) of body fat per week. The nurse knows that 0.45 kg (1 lb) of body fat is equal to 3,500 calories. The nurse should instruct the client to reduce his daily caloric intake by how many calories? (Round the answer to the nearest whole number. Use a leading zero if it applies. Do not use a trailing zero.)
Explanation
To lose 0.9 kg (2 lb) of body fat per week, the client needs to create a weekly caloric deficit of 7,000 calories (3,500 x 2).
This means that the client needs to consume 7,000 calories less than he burns in a week.
To achieve this, the client needs to reduce his daily caloric intake by 1,000 calories (7,000 / 7).
For example, if the client normally consumes 2,500 calories per day, he should reduce it to 1,500 calories per day.
A nurse is reinforcing teaching with a client who will undergo a colonoscopy the following week. Which of the following instructions should the nurse include?
Explanation
Choice A reason: Administering enemas 2 days before the procedure is not necessary for colonoscopy preparation. Enemas are usually given on the day of or the night before the procedure to empty the bowel and improve visibility.
Choice B reason: This is not necessary for a colonoscopy. A clear liquid diet for a shorter period, usually 12-24 hours, is sufficient.
Choice C reason: Expecting the provider to schedule another procedure to remove any polyps is not a valid instruction for colonoscopy preparation. Polyps are abnormal growths in the lining of the colon that can be benign or malignant. The provider can usually remove any polyps during the colonoscopy using a snare or a biopsy forceps.
Choice D reason: This is a standard bowel preparation instruction for colonoscopy to ensure a clear view of the colon during the procedure.
A nurse is reinforcing teaching with a client who is 24 hr postoperative following a total hip arthroplasty. Which of the following instructions should the nurse include in the teaching?
Explanation
Choice A reason: Performing range of motion by adducting the hip is an incorrect instruction for a client who had a total hip arthroplasty. Adduction is moving the leg toward the midline of the body, which can cause dislocation of the prosthesis. The nurse should instruct the client to perform range of motion by abducting (moving away from midline), flexing (bending), and extending (straightening) the hip as prescribed by physical therapy.
Choice B reason: Sitting in a straight-backed chair is a correct instruction for a client who had a total hip arthroplasty. This position helps to maintain proper alignment and stability of the hip joint and prevents excessive flexion or rotation that can cause dislocation. The nurse should also instruct the client to avoid crossing legs, bending forward more than 90 degrees, or twisting at the waist.
Choice C reason: Cleansing the surgical incision with hydrogen peroxide is an incorrect instruction for a client who had a total hip arthroplasty. Hydrogen peroxide is a harsh agent that can damage healthy tissue and delay healing. The nurse should instruct the client to cleanse the incision with mild soap and water or as directed by the provider and keep it dry and covered with sterile dressing.
Choice D reason: Applying moist heat to the incision while in bed is an incorrect instruction for a client who had a total hip arthroplasty. Moist heat can increase swelling, inflammation, and infection risk at the incision site. The nurse should instruct the client to apply ice packs or cold compresses to the incision as needed to reduce pain and swelling.
A nurse is reviewing vital signs obtained by an assistive personnel on a group of clients. The previous vital signs for each of the clients were obtained 4 hr earlier. Which of the following changes should the nurse identify as the priority finding?
Explanation
Choice A reason: Temperature change from 36.6° C (97.8° F) to 38.8° C (101.9° F) is a significant finding that indicates fever, which can be caused by infection, inflammation, or other conditions. However, this is not the priority finding because fever is usually a secondary response to an underlying problem and can be treated with antipyretics and fluids.
Choice B reason: Heart rate change from 110/min to 68/min is a notable finding that indicates bradycardia, which can be caused by medication, vagal stimulation, hypothermia, or cardiac dysfunction. However, this is not the priority finding because bradycardia may not be symptomatic or life-threatening unless it is accompanied by hypotension, chest pain, or altered mental status.
Choice C reason: Blood pressure change from 118/78 mm Hg to 86/50 mm Hg is the priority finding that indicates hypotension, which can be caused by blood loss, dehydration, shock, or medication. Hypotension can impair tissue perfusion and oxygenation and lead to organ failure and death if not corrected promptly. The nurse should assess the client for signs of shock, such as tachycardia, tachypnea, pallor, diaphoresis, or confusion, and initiate interventions to restore blood pressure and circulation.
Choice D reason: Respiratory rate change from 12/min to 20/min is a minor finding that indicates tachypnea, which can be caused by anxiety, pain, fever, or respiratory distress. However, this is not the priority finding because tachypnea may be a compensatory mechanism to increase oxygen delivery or eliminate carbon dioxide and may not affect gas exchange or acid-base balance unless it is severe or prolonged.
You just viewed 10 questions out of the 78 questions on the ATI PN Adult Medical Surgical 2020 with NGN Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



