The patient weighing 147 pounds with septic shock has a BP of 70/46 mm Hg, pulse 136, respirations 30, temperature 104° F, and blood glucose 391 mg/dL. Which intervention red by the health care provider should the nurse implement first?
Give a 2000mL normal saline bolus
Start insulin drip to maintain blood glucose at 110 to 150 mg/dL.
Give acetaminophen (Tylenol) 650 mg rectally.
Give prescribed Antibiotics
Start norepinephrine (Levophed) to keep systolic blood pressure >90 mm Hg.
The Correct Answer is D
In septic shock, prompt administration of antibiotics is crucial in order to target the underlying infection and prevent further progression of the septic process. Antibiotics help to eradicate the causative organisms and reduce the bacterial load, which can help improve patient outcomes.
While all the options mentioned are important interventions in the management of septic shock, initiating antibiotic therapy is considered a priority in order to address the underlying infection and prevent sepsis-related complications.
A. Giving a 2000 mL normal saline bolus in (option A) is incorrect because: Fluid resuscitation is important in septic shock to restore intravascular volume, but antibiotic therapy takes precedence as it directly targets the underlying infection.
B. Starting an insulin drip to maintain blood glucose at 110 to 150 mg/dL in (option B) is incorrect because Glycemic control is important in septic shock, but it is not the first priority compared to addressing the infection.
C. Giving acetaminophen (Tylenol) 650 mg rectally in (option C) is incorrect because Antipyretic medications can help reduce fever, but they do not address the underlying infection or stabilize the patient's condition.
E. Starting norepinephrine (Levophed) to keep systolic blood pressure >90 mm Hg in (option E) is incorrect because: Vasopressor support may be necessary in septic shock to maintain adequate blood pressure, but initiating antibiotics takes priority in order to address the underlying infection.
Therefore, in a patient with septic shock presenting with the given signs and symptoms, the nurse should first implement the intervention of giving the prescribed antibiotics to target the underlying infection.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Fresh frozen plasma (FFP) is a blood product that contains various clotting factors, including factors II, V, VII, VIII, IX, X, XI, and XIII. These clotting factors are essential for the normal coagulation process. In patients with shock, coagulation abnormalities can occur, and administration of FFP can help replenish the deficient clotting factors and restore proper coagulation function.
The other options mentioned are not the primary components replaced by fresh frozen plasma:
A. Red blood cells are in (option A) is incorrect because Red blood cells carry oxygen and are typically replaced by packed red blood cell transfusions in cases of significant blood loss or anemia. Fresh frozen plasma does not contain a significant amount of red blood cells.
C. Platelets in (option C) is incorrect because: Platelets play a role in blood clotting and are typically replaced by platelet transfusions in cases of thrombocytopenia or platelet dysfunction. Fresh frozen plasma may contain a small number of platelets but is not the primary source for platelet replacement.
D. White blood cells in (option D) is incorrect because White blood cells are part of the immune system and are not typically replaced using fresh frozen plasma. Fresh frozen plasma does not contain a significant amount of white blood cells.
Therefore, fresh frozen plasma is primarily administered to patients in shock to replace clotting factors and help restore proper coagulation function.
Correct Answer is C
Explanation
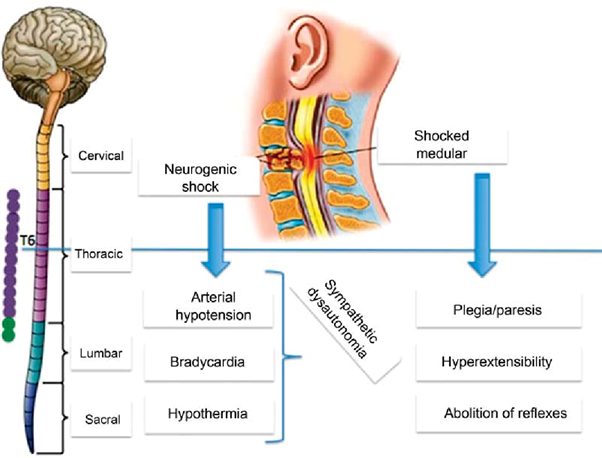
Neurogenic shock is a type of distributive shock that occurs due to the loss of sympathetic nervous system tone after a spinal cord injury or other traumatic brain injuries. This loss of sympathetic tone leads to vasodilation and decreased systemic vascular resistance, resulting in inadequate perfusion to vital organs.
One of the hallmark signs of neurogenic shock is bradycardia (a heart rate less than 60 beats/min) due to the unopposed parasympathetic activity. The parasympathetic system becomes dominant when sympathetic activity is impaired. Therefore, a heart rate of 48 beats/min in this patient suggests the possibility of neurogenic shock.
A. Cool, clammy skin in (option A) is incorrect because Cool, clammy skin is a characteristic of hypovolemic shock, where reduced blood volume leads to vasoconstriction to redirect blood flow to vital organs.
B. BP of 82/40 mm Hg in (option B) is incorrect because: Hypotension is a common finding in both neurogenic shock and hypovolemic shock. A low blood pressure reading alone does not specifically indicate neurogenic shock.
D. Shortness of breath in (option D) is incorrect because Shortness of breath is not specific to neurogenic shock but can occur in various types of shock, including hypovolemic shock. It may result from inadequate oxygenation or impaired respiratory function due to the underlying condition or associated injuries.
Therefore, the heart rate of 48 beats/min suggests the possibility of neurogenic shock in addition to hypovolemic shock in this patient.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
