A 29-year-old female patient is admitted to the emergency department with two of the systemic inflammatory response syndrome variables: temperature of 101.2 °F and 14,000 per μL white blood cell count. Which intervention from the sepsis resuscitation bundle does the nurse initiate?
Cooling baths
Broad-spectrum antibiotics
Blood transfusion
NPO status
The Correct Answer is B
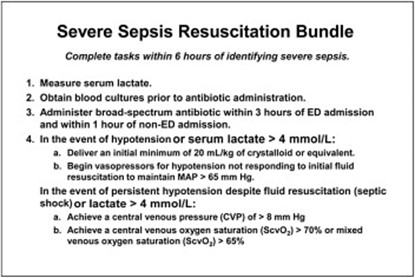
The patient's symptoms of fever and elevated white blood cell count suggest a potential infection and sepsis. Broad-spectrum antibiotics should be initiated promptly to cover a wide range of possible pathogens until further diagnostic tests and identification of the specific causative agent are obtained. Early administration of appropriate antibiotics is crucial in sepsis management to target the suspected infection and improve patient outcomes.
A. Cooling baths in (option A) is incorrect because: Cooling baths are typically used in the management of hyperthermia or specific conditions like heatstroke. While the patient has an elevated temperature, it is likely due to the systemic inflammatory response rather than solely hyperthermia.
C. Blood transfusion in (option C) is incorrect because Blood transfusion may be required in certain cases of sepsis if there is evidence of significant anemia or active bleeding. However, based on the information provided, there is no immediate indication of a blood transfusion.
D. NPO status in (option D) is incorrect because NPO status (nothing by mouth) is a general precautionary measure used in various situations, such as prior to surgery or to manage gastrointestinal complications. It is not a specific intervention in the sepsis resuscitation bundle.
Therefore, the nurse should initiate the intervention of administering broad-spectrum antibiotics in this scenario.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["21"]
Explanation
flow rate for an infusion= (Volume in mL * Drop factor) / Time in minutes.
volume of the infusion bag is 250 mL, the drop factor is 10 gtts/mL, and the time is 2 hours, which is 120 minutes.
(250 mL * 10 gtts/mL) / 120 minutes = 2500 gtts / 120 minutes ≈ 20.83 gtts/minute. Therefore, the nurse should run the infusion at a rate of approximately 21 drops per minute to deliver 1 unit of packed red blood cells over the 2-hour period.
Correct Answer is B
Explanation
Lactate is a by-product of anaerobic metabolism that accumulates when there is insufficient oxygen supply to meet cellular metabolic demands. In the context of severe tissue hypoxia, such as in septic shock, the body may resort to anaerobic metabolism, leading to increased lactate production and elevated lactate levels in the blood.
Elevated lactate levels, typically above 4.0 mmol/L, are indicative of tissue hypoxia and inadequate oxygenation at the cellular level. Higher lactate levels, such as 9.0 mmol/L, suggest more severe tissue hypoxia and increased anaerobic metabolism.
A. Partial thromboplastin time (PTT) 64 seconds in (option A) is incorrect because: PTT is a laboratory test that evaluates the intrinsic pathway of the coagulation cascade. While coagulation abnormalities may occur in septic shock, PTT alone does not specifically indicate severe tissue hypoxia.
C. Potassium 2.8 mEq/L (2.8 mmol/L) (option C) is incorrect because Low potassium levels (hypokalemia) can be a concern in septic shock, but it does not directly indicate severe tissue hypoxia.
D. PaCO2 58 mm Hg in (option D) is incorrect because: PaCO2 refers to the partial pressure of carbon dioxide in arterial blood and is a measure of the respiratory status. While an elevated PaCO2 can be a sign of respiratory acidosis, it is not specific to severe tissue hypoxia.
Therefore, in a critically ill patient with septic shock, an elevated lactate level, such as 9.0 mmol/L, indicates severe tissue hypoxia and inadequate oxygenation at the cellular level
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
