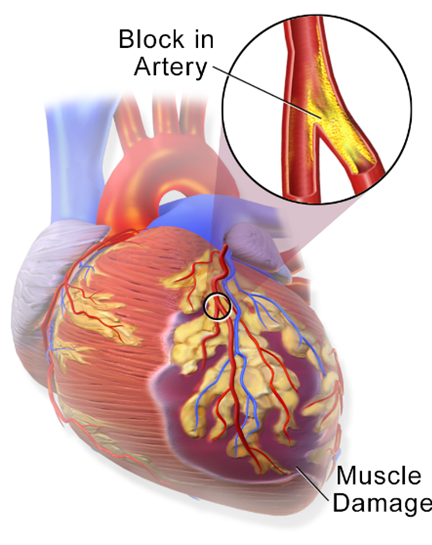
The nurse obtains a monitor strip on a patient who has had a myocardial infarction and makes the following analysis: P wave not apparent, ventricular rate 196, R-R interval regular, P-R interval not measurable, QRS complex wide and distorted, QRS duration 0.18 second. The nurse interprets the patient's cardiac rhythm as;
ventricular tachycardia.
atrial fibrillation.
atrial tachycardia.
ventricular fibrillation.
The Correct Answer is A
The characteristics described in the monitor strip analysis suggest ventricular tachycardia. The absence of a visible P wave and the wide and distorted QRS complex indicates that the electrical impulse is originating in the ventricles rather than the atria. The ventricular rate of 196 and regular R-R intervals further support the diagnosis of ventricular tachycardia.
B. Atrial fibrillation in (option B) is incorrect because it is characterized by irregularly irregular R-R intervals and the absence of discernible P waves. The QRS complex is typically narrow
C. Atrial tachycardia in (option C) is incorrect because it would have a rapid atrial rate with regular R-R intervals, and P waves may or may not be discernible. The QRS complex is typically narrow.
D. Ventricular fibrillation in (option D) is incorrect because it would present as a chaotic, rapid, and irregular electrical activity with no discernible P waves, QRS complexes, or regular R-R intervals. It is a life-threatening emergency that requires immediate defibrillation.
Therefore, based on the provided information, the nurse would interpret the patient's cardiac rhythm as ventricular tachycardia. However, it is important to note that an accurate interpretation should be made by a qualified healthcare professional, and the patient's clinical context should also be considered.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
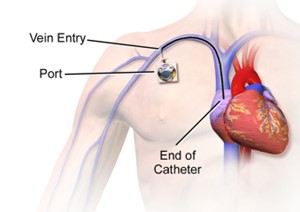
Central venous pressure (CVP) is a measurement of the pressure in the central veins, which reflects the blood volume and right-sided cardiac function. High CVP readings may indicate fluid overload or impaired cardiac function, and intervention is necessary to address the underlying cause.
Administering IV diuretic medications can help reduce fluid volume by increasing urine output and promoting fluid elimination. By removing excess fluid, the diuretic medications can help lower the CVP and alleviate the high pressures.
The other options mentioned are not the anticipated actions for addressing high CVP:
A. Increasing the IV fluid infusion rate in (option A) is incorrect because: If the CVP is already indicating high pressures, increasing the IV fluid infusion rate would further contribute to fluid overload and exacerbate the problem. This action would not be appropriate for high CVP readings.
C. Elevating the head of the patient's bed to 45 degrees in (option C) is incorrect because Positioning the patient with the head of the bed elevated is commonly done to prevent complications such as aspiration or improve respiratory function. While it may have other benefits, it does not directly address the high CVP.
D. Documenting the CVP and continuing to monitor in (option D) is incorrect because Documenting the CVP and continuing to monitor is important for ongoing assessment and evaluation. However, in the presence of high CVP readings, intervention is necessary to address the underlying issue rather than solely documenting and monitoring.
Therefore, when a patient's CVP monitor indicates high pressures following surgery, the nurse would anticipate administering IV diuretic medications to help reduce fluid volume and lower the CVP.
Correct Answer is C
Explanation
Urine output is an essential indicator of renal perfusion and overall fluid status. In a patient in shock, maintaining an adequate urine output is a crucial goal of fluid resuscitation. A urine output of 0.5 to 1 mL/kg/hour is generally considered adequate in adults. The given value of 35 ml over the last hour suggests that the patient is producing urine, which indicates that fluid resuscitation is effective in restoring perfusion to the kidneys.
A. The patient's mean arterial pressure (MAP) is 50 mm Hg in (option A) is incorrect because While mean arterial pressure is an important hemodynamic parameter, a single value alone may not provide a comprehensive assessment of the patient's response to fluid resuscitation.
B. The patient's GCS score is 9 in (option B) is incorrect because The Glasgow Coma Scale (GCS) assesses the level of consciousness and neurological function but does not directly reflect fluid resuscitation effectiveness.
D. The patient's hemoglobin is within normal limits: (option D) is incorrect because Haemoglobin levels are important for assessing oxygen-carrying capacity but do not directly indicate the effectiveness of fluid resuscitation.
Therefore, the nurse can evaluate that fluid resuscitation for a 70 kg patient in shock is effective by observing a urine output of 35 ml over the last hour.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
