The nurse is caring for a patient receiving a continuous norepinephrine (Levophed) IV infusion. Which patient assessment information indicates that the infusion rate may be too high?
Mean arterial pressure is 55 mm Hg.
Systemic vascular resistance (SVR) is elevated.
Pulmonary artery wedge pressure (PAWP) is low.
Heart rate is 58 beats/min.
The Correct Answer is D
Norepinephrine is a potent vasoconstrictor and inotropic agent commonly used to increase blood pressure in cases of hypotension or shock. However, if the infusion rate is too high, it can lead to excessive vasoconstriction and potentially compromise organ perfusion.
A heart rate of 58 beats/min suggests bradycardia, which can be an indication of excessive vasoconstriction caused by a high dose or rate of norepinephrine infusion. Excessive vasoconstriction can reduce cardiac output and worsen tissue perfusion.
A. Mean arterial pressure is 55 mm Hg in (option A) is incorrect because A mean arterial pressure of 55 mm Hg may be within an acceptable range for a patient receiving norepinephrine infusion, depending on the patient's baseline blood pressure and clinical condition.
B. Systemic vascular resistance (SVR) is elevated in (option B) is incorrect because An elevated SVR indicates increased peripheral vascular resistance and can be a desired effect of norepinephrine infusion to improve blood pressure and perfusion.
C. Pulmonary artery wedge pressure (PAWP) is low in (option C) which is incorrect because A low PAWP may indicate decreased left ventricular preload, which can be a desired effect of norepinephrine infusion to reduce fluid overload in certain clinical conditions.
It is important for the nurse to carefully monitor the patient's hemodynamic parameters, including blood pressure, heart rate, and organ perfusion when titrating norepinephrine infusion to ensure optimal dosing and minimize potential adverse effects. If concerns arise regarding the infusion rate, the healthcare provider should be promptly notified for further evaluation and adjustment of the treatment plan.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Septic shock is characterized by inadequate tissue perfusion and hypotension, which can lead to organ dysfunction and failure. The administration of intravenous fluids, such as a normal saline bolus, is the initial priority in the management of septic shock to restore intravascular volume and improve perfusion.
A. Draw an arterial blood gas (ABG) in (option A) is incorrect because: ABG may be ordered to assess the patient's acid-base status and oxygenation, but addressing hypotension and restoring perfusion through fluid administration takes priority.
B. Start insulin drip to maintain blood glucose at 150 mg/dl or lower in (option B) is incorrect because: Hyperglycaemia is commonly observed in critically ill patients, including those with septic shock. While controlling blood glucose is important, it is not the immediate priority compared to addressing hypotension and restoring intravascular volume.
D. Titrate norepinephrine (Levophed) to keep mean arterial pressure (MAP) greater than 65 mm Hg in (option D) is incorrect because: Norepinephrine is a vasopressor medication used to increase blood pressure and perfusion in septic shock. While it may be necessary for the management of septic shock, fluid resuscitation should be initiated first to optimize intravascular volume before starting vasopressors.
Therefore, the first order that the nurse should accomplish in this scenario is to give a normal saline bolus IV of 30 mL/kg to address the hypotension and restore intravascular volume.
Correct Answer is A
Explanation
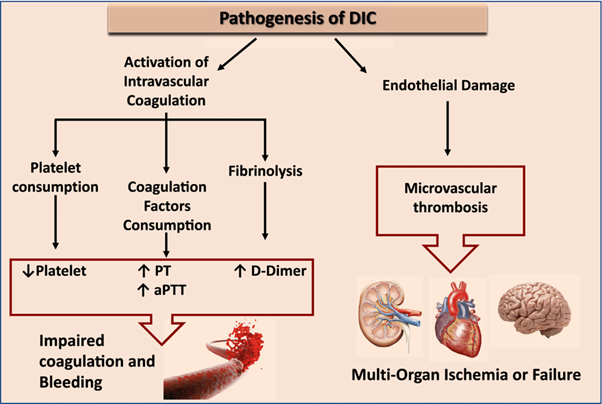
Disseminated intravascular coagulation (DIC) is a condition characterized by both widespread activation of the coagulation system and excessive clotting, leading to the consumption of clotting factors and platelets. This results in a prothrombotic state, which can lead to organ dysfunction and bleeding manifestations.
Elevated D-dimer levels are a characteristic finding in DIC. D-dimer is a fibrin degradation product that is elevated when there is excessive fibrin formation and breakdown. Elevated D-dimer indicates ongoing fibrinolysis and activation of the clotting system.
B. Decreased prothrombin time in (option B) is incorrect because: DIC is characterized by consumption of clotting factors, which can result in prolongation of the prothrombin time (PT) as well as other coagulation tests.
C. Decreased partial thromboplastin time in (option C) is incorrect because Similar to the prothrombin time, the partial thromboplastin time (PTT) can also be prolonged in DIC due to the consumption of clotting factors.
D. Elevated fibrinogen level in (option D) is incorrect because, In DIC, there is consumption of fibrinogen along with other clotting factors. Therefore, elevated fibrinogen levels are not consistent with the pathophysiology of DIC.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
