A 40-year-old female patient with massive trauma and possible spinal cord injury is admitted to the emergency department (ED). The nurse suspects that the patient may be experiencing neurogenic shock in addition to hypovolemic shock, based on which one of the following?
Cool, clammy skin.
BP of 82/40 mm Hg.
Heart rate of 48 beats/min.
Shortness of breath.
The Correct Answer is C
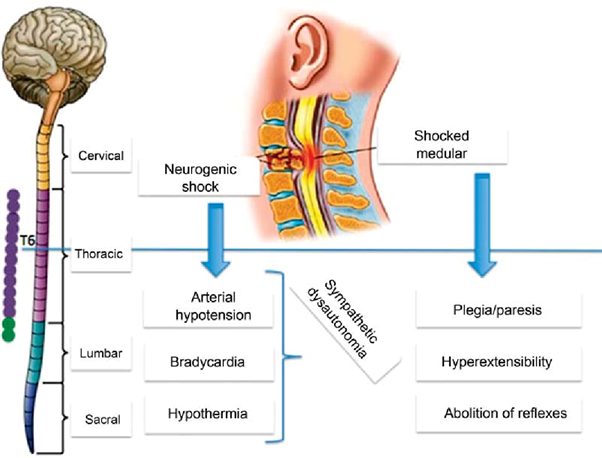
Neurogenic shock is a type of distributive shock that occurs due to the loss of sympathetic nervous system tone after a spinal cord injury or other traumatic brain injuries. This loss of sympathetic tone leads to vasodilation and decreased systemic vascular resistance, resulting in inadequate perfusion to vital organs.
One of the hallmark signs of neurogenic shock is bradycardia (a heart rate less than 60 beats/min) due to the unopposed parasympathetic activity. The parasympathetic system becomes dominant when sympathetic activity is impaired. Therefore, a heart rate of 48 beats/min in this patient suggests the possibility of neurogenic shock.
A. Cool, clammy skin in (option A) is incorrect because Cool, clammy skin is a characteristic of hypovolemic shock, where reduced blood volume leads to vasoconstriction to redirect blood flow to vital organs.
B. BP of 82/40 mm Hg in (option B) is incorrect because: Hypotension is a common finding in both neurogenic shock and hypovolemic shock. A low blood pressure reading alone does not specifically indicate neurogenic shock.
D. Shortness of breath in (option D) is incorrect because Shortness of breath is not specific to neurogenic shock but can occur in various types of shock, including hypovolemic shock. It may result from inadequate oxygenation or impaired respiratory function due to the underlying condition or associated injuries.
Therefore, the heart rate of 48 beats/min suggests the possibility of neurogenic shock in addition to hypovolemic shock in this patient.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
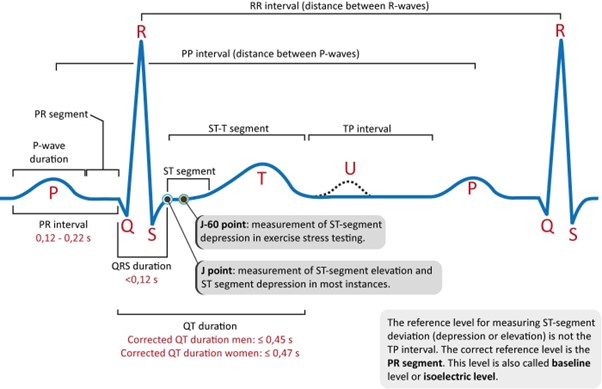
The QTc (corrected QT) interval is a measure of the time it takes for the ventricles to depolarize and repolarize during a cardiac cycle. It is corrected for heart rate (HR) to account for variations in the cardiac cycle length.
The normal range for the QTc interval varies depending on the calculation method used but generally falls within 0.36 to 0.44 seconds. In the given options, the range of 0.33 to 0.47 seconds for the QTc interval is wider than the normal range, suggesting a prolonged QTc interval, which can be indicative of a potential risk for arrhythmias, including ventricular tachycardia and torsades de pointes.
B. QT interval that varies with HR in (option B) is normal because The QT interval alone can vary with heart rate, and this is considered a normal physiological adaptation.
C. QRS interval <0.12 seconds in (option C) is normal because The QRS interval represents the time it takes for ventricular depolarization and is normally less than 0.12 seconds.
D. PR interval 0.12 to 0.24 seconds in (option D) is normal because The PR interval represents the time it takes for atrial depolarization and conduction through the AV node. The normal range is typically 0.12 to 0.20 seconds.
Correct Answer is ["A","B","D","E"]
Explanation
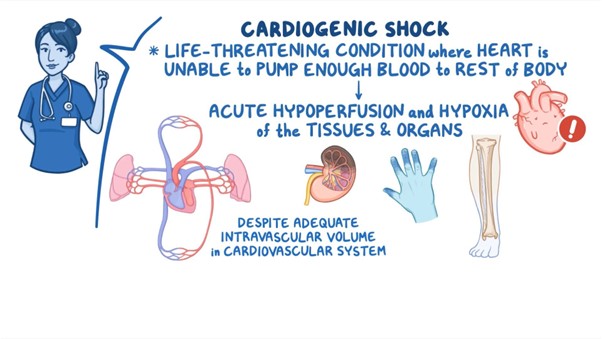
A. Narrowed pulse pressure: In cardiogenic shock, the cardiac output is compromised, resulting in reduced stroke volume and subsequent narrowed pulse pressure. The pulse pressure is the difference between systolic and diastolic blood pressure.
B. Tachycardia: Tachycardia is a compensatory response in cardiogenic shock, as the body attempts to increase cardiac output to maintain tissue perfusion despite decreased stroke volume. Increased heart rate is a common finding in this condition.
D. Pulmonary congestion: Cardiogenic shock is often associated with impaired left ventricular function, leading to an inadequate pump mechanism. This can result in fluid accumulation and congestion in the pulmonary circulation, leading to pulmonary edema and congestion. Patients may experience symptoms such as dyspnea, crackles on lung auscultation, and increased work of breathing.
E. Elevated pulmonary artery wedge pressure (PAWP): PAWP is a measurement obtained during invasive hemodynamic monitoring. In cardiogenic shock, the impaired left ventricular function leads to increased left atrial pressure, which is reflected by an elevated PAWP. Elevated PAWP indicates increased fluid volume and congestion in the left side of the heart.
C. Elevated SBP in (option C) is incorrect because Elevated systolic blood pressure (SBP) is not a typical finding in cardiogenic shock. Instead, hypotension or decreased blood pressure is commonly observed due to reduced cardiac output.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
