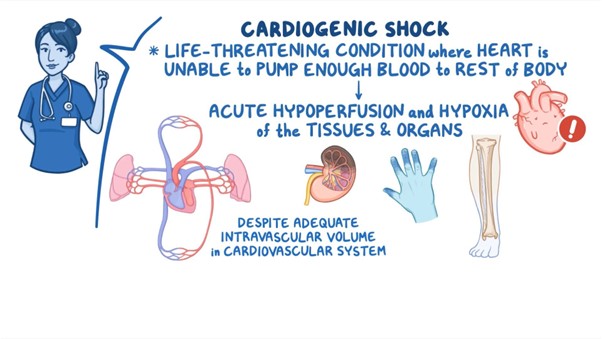
The cardiac ICU nurse is assessing a patient who is in cardiogenic shock. Which hemodynamic manifestations and/or signs and symptoms do the nurse expect? Select all that apply.
Narrowed pulse pressure.
Tachycardia.
Elevated SBP.
Pulmonary congestion.
Pulmonary artery wedge pressure
Correct Answer : A,B,D,E
A. Narrowed pulse pressure: In cardiogenic shock, the cardiac output is compromised, resulting in reduced stroke volume and subsequent narrowed pulse pressure. The pulse pressure is the difference between systolic and diastolic blood pressure.
B. Tachycardia: Tachycardia is a compensatory response in cardiogenic shock, as the body attempts to increase cardiac output to maintain tissue perfusion despite decreased stroke volume. Increased heart rate is a common finding in this condition.
D. Pulmonary congestion: Cardiogenic shock is often associated with impaired left ventricular function, leading to an inadequate pump mechanism. This can result in fluid accumulation and congestion in the pulmonary circulation, leading to pulmonary edema and congestion. Patients may experience symptoms such as dyspnea, crackles on lung auscultation, and increased work of breathing.
E. Elevated pulmonary artery wedge pressure (PAWP): PAWP is a measurement obtained during invasive hemodynamic monitoring. In cardiogenic shock, the impaired left ventricular function leads to increased left atrial pressure, which is reflected by an elevated PAWP. Elevated PAWP indicates increased fluid volume and congestion in the left side of the heart.
C. Elevated SBP in (option C) is incorrect because Elevated systolic blood pressure (SBP) is not a typical finding in cardiogenic shock. Instead, hypotension or decreased blood pressure is commonly observed due to reduced cardiac output.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["9"]
Explanation
-
Doseinmcg/min=2mcg/kg/min×60kg=120mcg/min
Convert this to mg/min since the concentration is in mg:
120mcg/min=0.12mg/min120 \text{ mcg/min} = 0.12 \text{ mg/min}120mcg/min=0.12mg/min
-
Determine the concentration of Dopamine:
- Total amount of Dopamine: 200 mg in 250 mL of saline
- Concentration:
Concentration=200mg250mL=0.8mg/mL\text{Concentration} = \frac{200 \text{ mg}}{250 \text{ mL}} = 0.8 \text{ mg/mL}Concentration=250mL200mg=0.8mg/mL
-
Calculate the pump rate in mL/min:
To find the rate in mL/min needed to deliver 0.12 mg/min:
Pumprate=Desireddose(mg/min)Concentration(mg/mL)\text{Pump rate} = \frac{\text{Desired dose (mg/min)}}{\text{Concentration (mg/mL)}}Pumprate=Concentration(mg/mL)Desireddose(mg/min)
Pumprate=0.12mg/min0.8mg/mL=0.15mL/min\text{Pump rate} = \frac{0.12 \text{ mg/min}}{0.8 \text{ mg/mL}} = 0.15 \text{ mL/min}Pumprate=0.8mg/mL0.12mg/min=0.15mL/min
-
Convert the pump rate to mL/hour:
Multiply by 60 to convert from mL/min to mL/hour:
Pumprate=0.15mL/min×60min/hour=9mL/hour\text{Pump rate} = 0.15 \text{ mL/min} \times 60 \text{ min/hour} = 9 \text{ mL/hour}Pumprate=0.15mL/min×60min/hour=9mL/hour
So, you should set the pump to deliver Dopamine at a rate of 9 mL/hour.
Correct Answer is C
Explanation
Septic shock is a life-threatening condition characterized by severe infection, systemic inflammation, and inadequate tissue perfusion. In this critical situation, one of the initial priorities is to restore intravascular volume and improve tissue perfusion. Initiation of an intravenous line allows for the administration of fluids and other necessary medications to support the patient's hemodynamic stability.
While the other interventions mentioned are also important components of septic shock management, the immediate priority is to address hypotension and tissue hypoperfusion through fluid resuscitation:
A. Obtaining wound and blood cultures in (option A) is incorrect because: Cultures are important to identify the source and causative organisms of the infection. However, fluid resuscitation should take priority over obtaining cultures, as it is necessary to stabilize the patient's hemodynamics.
B. Removing or controlling potentially infected sources in (option B) is incorrect because: Identifying and controlling the source of infection is crucial in septic shock management to prevent further progression. However, initiating fluid resuscitation is more time-sensitive and should be prioritized.
D. Drawing blood for hematology and chemistry studies in (option D) is incorrect because Laboratory studies are important for evaluating organ function and guiding treatment. However, the immediate focus should be on fluid resuscitation to address the underlying hypoperfusion and stabilize the patient's condition.
Therefore, the intervention considered a priority when treating a patient who presents with septic shock is the initiation of an intravenous line and fluid administration to restore intravascular volume and improve tissue perfusion.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
