A 27-year-old male patient who has been involved in a motor vehicle crash is admitted to the emergency department with cool, clammy skin, tachypnoea, tachycardia, and hypotension. All of these orders are written. Which one will the nurse act on first?
Place the patient on a continuous cardiac monitor.
Administer oxygen at 100% per non-rebreather mask.
Insert two 14-gauge IV catheters.
Draw blood to type and crossmatch for transfusions.
The Correct Answer is B
In this scenario, the patient's signs and symptoms suggest a state of shock, which can be caused by various factors, such as hypovolemia, cardiac dysfunction, or systemic vasodilation. The first priority in managing a patient in shock is to ensure adequate oxygenation and tissue perfusion. Administering oxygen at 100% per non-rebreather mask helps improve oxygen delivery to the tissues and supports vital organ function.
A. Placing the patient on a continuous cardiac monitor in (option A) is incorrect because it is an important step to monitor the patient's heart rhythm and identify any abnormalities. However, providing oxygen should take priority to address the potential hypoxemia and tissue hypoperfusion.
C. Inserting two 14-gauge IV catheters in (option C) is incorrect because it is crucial for establishing large-bore access for fluid resuscitation and medication administration. While it is an important step, addressing oxygenation takes precedence.
D. Drawing blood to type and crossmatch for transfusions in (option D) is incorrect because it is an important step in managing a patient in shock who may require blood products. However, ensuring adequate oxygenation through oxygen administration is the immediate priority.
Therefore, the nurse should act first on the order to administer oxygen at 100% per non-rebreather mask to support the patient's oxygenation and tissue perfusion.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Septic shock is a life-threatening condition characterized by severe infection, systemic inflammation, and inadequate tissue perfusion. In this critical situation, one of the initial priorities is to restore intravascular volume and improve tissue perfusion. Initiation of an intravenous line allows for the administration of fluids and other necessary medications to support the patient's hemodynamic stability.
While the other interventions mentioned are also important components of septic shock management, the immediate priority is to address hypotension and tissue hypoperfusion through fluid resuscitation:
A. Obtaining wound and blood cultures in (option A) is incorrect because: Cultures are important to identify the source and causative organisms of the infection. However, fluid resuscitation should take priority over obtaining cultures, as it is necessary to stabilize the patient's hemodynamics.
B. Removing or controlling potentially infected sources in (option B) is incorrect because: Identifying and controlling the source of infection is crucial in septic shock management to prevent further progression. However, initiating fluid resuscitation is more time-sensitive and should be prioritized.
D. Drawing blood for hematology and chemistry studies in (option D) is incorrect because Laboratory studies are important for evaluating organ function and guiding treatment. However, the immediate focus should be on fluid resuscitation to address the underlying hypoperfusion and stabilize the patient's condition.
Therefore, the intervention considered a priority when treating a patient who presents with septic shock is the initiation of an intravenous line and fluid administration to restore intravascular volume and improve tissue perfusion.
Correct Answer is D
Explanation
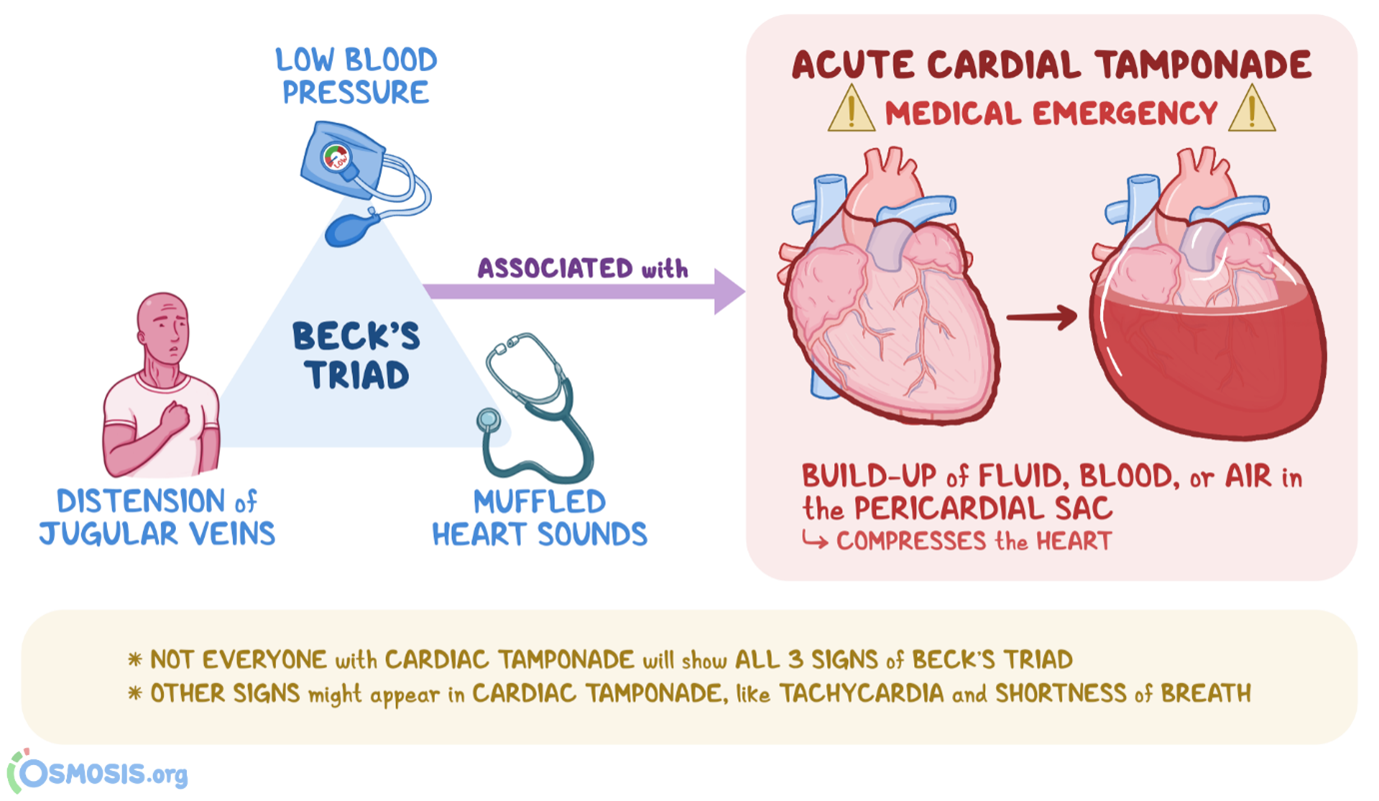
Beck's triad consists of three classic clinical manifestations that are suggestive of cardiac tamponade, which is the compression of the heart by accumulated fluid or blood within the pericardial sac. The three components of Beck's triad include:
A. Muffled heart tones in (option A) are incorrect because Cardiac tamponade can dampen or muffle heart sounds due to the presence of fluid or blood around the heart, which can impair sound transmission.
B. Marked hypotension in (option B) is incorrect because Cardiac tamponade can cause decreased cardiac output, leading to hypotension, which is characterized by low blood pressure.
C. Distended jugular veins in (option C) is incorrect because Elevated venous pressure resulting from impaired filling and elevated right-sided heart pressures can lead to jugular vein distension, which is commonly seen in cardiac tamponade.
However, widening pulse pressure (the difference between systolic and diastolic blood pressure) is not typically part of Beck's triad. Widening pulse pressure is associated with her conditions such as aortic regurgitation, hyperthyroidism, or conditions involving increased stroke volume, rather than cardiac tamponade specifically.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
