A student is caring for a patient who suffered massive blood loss after trauma. How does the student correlate the blood loss with the patient's mean arterial pressure (MAP)?
It causes vasoconstriction and increased MAP.
Lower blood volume lowers MAP.
It raises cardiac output and MAP.
There is no direct correlation to MAP.
The Correct Answer is B
Mean arterial pressure (MAP) is a measure of the average pressure within the arteries during one cardiac cycle. It represents the perfusion pressure that drives blood flow to organs and tissues. MAP is calculated using the formula:
MAP = Diastolic blood pressure + 1/3 (Systolic blood pressure - Diastolic blood pressure)
Blood loss, particularly in cases of significant hemorrhage, leads to a decrease in blood volume. When blood volume decreases, there is less circulating blood available to generate pressure within the arterial system. This reduction in blood volume results in decreased MAP.
Therefore, in the case of massive blood loss after trauma, the student can correlate it with a lower blood volume, which in turn leads to a lower MAP. The decrease in blood volume reduces the perfusion pressure, compromising organ and tissue perfusion
A. It causes vasoconstriction and increased MAP in (option A) is incorrect because: While vasoconstriction can occur as a compensatory mechanism to maintain blood pressure, it does not necessarily lead to an increased MAP in the context of significant blood loss.
C. It raises cardiac output and MAP in (option C) is incorrect because Blood loss typically leads to a reduction in cardiac output due to decreased blood volume. Therefore, it does not raise cardiac output and MAP.
D. There is no direct correlation to MAP in (option D) is incorrect because: There is indeed a direct correlation between blood loss and MAP. As blood volume decreases, MAP decreases as well.
Therefore, the correct correlation between blood loss and MAP is that lower blood volume lowers MAP.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Heart rate: 72 beats per minute Stroke volume: 90 mL/contraction
Cardiac output = Heart rate × Stroke volume
Cardiac output = 72 beats/minute × 90 mL/contraction
To simplify the calculation, you can convert the units:
72 beats/minute × 90 mL/contraction = (72 × 90) beats/minute × mL/contraction
Now, perform the multiplication:
72 × 90 = 6,480
Therefore, the cardiac output is 6,480 mL per minute.
The correct answer is:
C. 6,480 mL
Correct Answer is A
Explanation
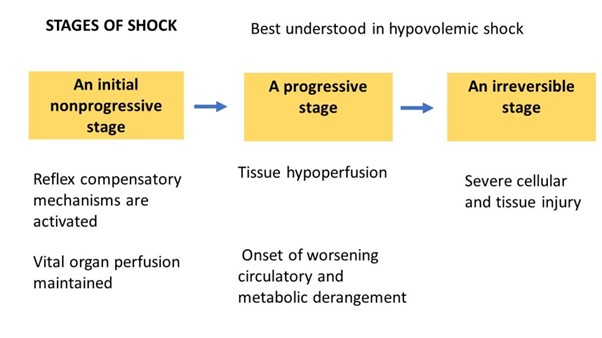
In the early stage of septic shock, the body initiates compensatory mechanisms to combat the infection and restore adequate tissue perfusion. Tachypnoea (rapid breathing) and tachycardia (elevated heart rate) are common early signs of septic shock.
Tachypnoea occurs as a response to increased metabolic demand and to compensate for impaired oxygenation and tissue perfusion. Tachycardia is the body's attempt to maintain cardiac output and compensate for decreased blood pressure.
B. Pallor and cool skin in (option B) is incorrect because Pallor and cool skin can occur in later stages of septic shock when perfusion to the peripheral tissues is compromised. However, they are not specific to the early stage.
C. Blood pressure 84/50 mm Hg in (option C) is incorrect because A blood pressure reading of 84/50 mm Hg indicates hypotension, which is typically seen in later stages of septic shock. In the early stage, blood pressure may still be within normal or slightly decreased range.
D. Respiratory acidosis in (optionD) is incorrect because: Respiratory acidosis refers to an imbalance in acid-base status and is not specific to the early stage of septic shock. Acid-base disturbances may occur at any stage of shock but are not indicative of the early stage.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
