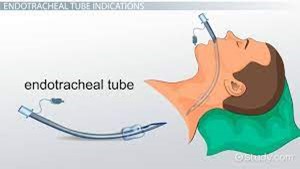
To verify the correct placement of an endotracheal tube (ET) after insertion, the best initial action by the nurse is to:
auscultate for the presence of bilateral breath sounds.
Use an end-tidal C02 monitor to check for placement in the trachea.
Observe the chest for symmetrical movement with ventilation.
Obtain a portable chest radiograph to check tube placement.
The Correct Answer is C
The nurse should listen over both lung fields to ensure that air entry is present bilaterally, indicating that the tube is correctly positioned in the trachea. This comes after observing chest movements.
B. Using an end-tidal CO2 monitor to check for placement in the trachea in (option B) is incorrect because End-tidal CO2 monitoring can provide confirmation of correct tube placement in the trachea by detecting exhaled CO2 levels. However, it requires additional equipment and setup, which may not be readily available at the bedside or immediately accessible.
C. Observing the chest for symmetrical movement with ventilation is the initial action after placing an endotracheal tube.
D. Obtaining a portable chest radiograph to check tube placement (option D) is incorrect because Chest radiographs are commonly used to confirm endotracheal tube placement, especially for long-term confirmation or if there are concerns about placement. However, obtaining a portable chest radiograph may involve delays and is not the initial action to be taken for immediate verification.
Therefore, the best initial action by the nurse to verify the correct placement of an endotracheal tube (ET) after insertion is to auscultate for the presence of bilateral breath sounds.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is ["9"]
Explanation
-
Doseinmcg/min=2mcg/kg/min×60kg=120mcg/min
Convert this to mg/min since the concentration is in mg:
120mcg/min=0.12mg/min120 \text{ mcg/min} = 0.12 \text{ mg/min}120mcg/min=0.12mg/min
-
Determine the concentration of Dopamine:
- Total amount of Dopamine: 200 mg in 250 mL of saline
- Concentration:
Concentration=200mg250mL=0.8mg/mL\text{Concentration} = \frac{200 \text{ mg}}{250 \text{ mL}} = 0.8 \text{ mg/mL}Concentration=250mL200mg=0.8mg/mL
-
Calculate the pump rate in mL/min:
To find the rate in mL/min needed to deliver 0.12 mg/min:
Pumprate=Desireddose(mg/min)Concentration(mg/mL)\text{Pump rate} = \frac{\text{Desired dose (mg/min)}}{\text{Concentration (mg/mL)}}Pumprate=Concentration(mg/mL)Desireddose(mg/min)
Pumprate=0.12mg/min0.8mg/mL=0.15mL/min\text{Pump rate} = \frac{0.12 \text{ mg/min}}{0.8 \text{ mg/mL}} = 0.15 \text{ mL/min}Pumprate=0.8mg/mL0.12mg/min=0.15mL/min
-
Convert the pump rate to mL/hour:
Multiply by 60 to convert from mL/min to mL/hour:
Pumprate=0.15mL/min×60min/hour=9mL/hour\text{Pump rate} = 0.15 \text{ mL/min} \times 60 \text{ min/hour} = 9 \text{ mL/hour}Pumprate=0.15mL/min×60min/hour=9mL/hour
So, you should set the pump to deliver Dopamine at a rate of 9 mL/hour.
Correct Answer is A
Explanation
The increased respiratory rate and pulse rate can be indicators of physiological changes or potential complications in the patient's condition. These changes may suggest alterations in tissue perfusion or other underlying issues that require further assessment.
Assessing the patient's tissue perfusion includes evaluating additional vital signs, such as blood pressure, oxygen saturation, and capillary refill time. Assessing skin color, temperature, and moisture, as well as peripheral pulses, can also provide important information regarding tissue perfusion.
B. Pain medication (option B) is incorrect because the increased respiratory and pulse rates could also indicate other factors that require assessment before administering pain medication.
C. Documenting the findings in the patient's chart (option C) is incorrect because it should not be the primary action at this point. Assessing the patient's condition and determining appropriate interventions take priority.
D. Increasing the rate of the patient's IV infusion (option D) is incorrect because may not be the most appropriate action without further assessment. The patient's increased respiratory and pulse rates may not necessarily be related to hydration status, and it is important to assess the patient comprehensively before making changes to the IV infusion rate.
Therefore, the best action by the nurse in this situation is to further assess the patient's tissue perfusion to gather more information and determine the appropriate course of action.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
