To determine the effectiveness of medications that a patient has received to reduce left ventricular afterload, which hemodynamic parameter will the nurse monitor?
Pulmonary artery wedge pressure (PAWP)
Systemic vascular resistance (SVR)
Pulmonary vascular resistance (PVR)
Central venous pressure (CVP)
The Correct Answer is B
Systemic vascular resistance represents the resistance to blood flow in the systemic circulation. It is an important indicator of afterload, which is the force against which the left ventricle must pump to eject blood into the systemic circulation. By monitoring the changes in SVR, the nurse can assess the impact of medications aimed at reducing left ventricular afterload.
A. Pulmonary artery wedge pressure (PAWP) in (option A) is incorrect because: PAWP is a measure of left ventricular preload and reflects the pressure within the left atrium and left ventricle at end-diastole. It is not specifically related to afterload reduction.
C. Pulmonary vascular resistance (PVR) in (option C) is incorrect because: PVR represents the resistance to blood flow in the pulmonary circulation. It is not directly related to left ventricular afterload.
D. Central venous pressure (CVP) in (option D) is incorrect because: CVP reflects the pressure in the right atrium and is an indicator of right-sided cardiac function. It is not specifically related to left ventricular afterload reduction.
Therefore, to assess the effectiveness of medications in reducing left ventricular afterload, the nurse should monitor the systemic vascular resistance (SVR).
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
The sepsis resuscitation bundle typically includes the administration of intravenous fluids to restore adequate perfusion and address hypovolemia. The initial fluid of choice is often the crystalloid solution, such as Lactated Ringers (LR), and the recommended initial fluid bolus is 30 ml/kg. This intervention aims to optimize intravascular volume and improve tissue perfusion.
A. Cooling baths in (option A) is incorrect because they may be used in the management of hyperthermia or fever, but they are not specific interventions in the sepsis resuscitation bundle.
B. Blood transfusion in (option B) is incorrect it may be necessary in certain cases of sepsis, such as severe anemia or hypovolemia, but it is not a routine intervention in the sepsis resuscitation bundle based solely on the provided information.
D. NPO status (nothing by mouth) in (option D) is incorrect because it is not a specific intervention in the sepsis resuscitation bundle. It may be indicated in certain cases, such as when surgery is required or if there is a risk of aspiration, but it does not directly address the sepsis-related variables mentioned.
It is important to note that the specific management of sepsis may vary based on the patient's individual condition, clinical presentation, and healthcare provider's orders.
Correct Answer is ["A","B","D","E"]
Explanation
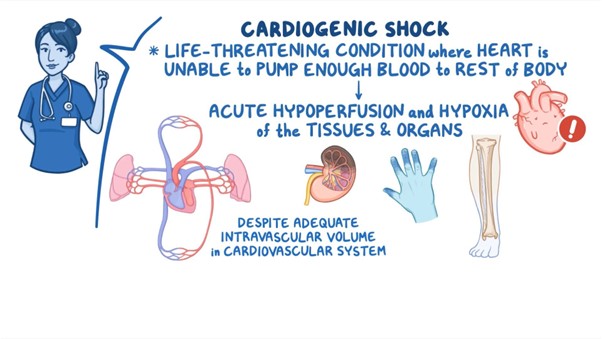
A. Narrowed pulse pressure: In cardiogenic shock, the cardiac output is compromised, resulting in reduced stroke volume and subsequent narrowed pulse pressure. The pulse pressure is the difference between systolic and diastolic blood pressure.
B. Tachycardia: Tachycardia is a compensatory response in cardiogenic shock, as the body attempts to increase cardiac output to maintain tissue perfusion despite decreased stroke volume. Increased heart rate is a common finding in this condition.
D. Pulmonary congestion: Cardiogenic shock is often associated with impaired left ventricular function, leading to an inadequate pump mechanism. This can result in fluid accumulation and congestion in the pulmonary circulation, leading to pulmonary edema and congestion. Patients may experience symptoms such as dyspnea, crackles on lung auscultation, and increased work of breathing.
E. Elevated pulmonary artery wedge pressure (PAWP): PAWP is a measurement obtained during invasive hemodynamic monitoring. In cardiogenic shock, the impaired left ventricular function leads to increased left atrial pressure, which is reflected by an elevated PAWP. Elevated PAWP indicates increased fluid volume and congestion in the left side of the heart.
C. Elevated SBP in (option C) is incorrect because Elevated systolic blood pressure (SBP) is not a typical finding in cardiogenic shock. Instead, hypotension or decreased blood pressure is commonly observed due to reduced cardiac output.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
