A 66-year-old female patient in septic shock has received fluid resuscitation, but their mean arterial pressure (MAP) is 52 mmHg. The nurse anticipates the administration of which one of the following?
Nitroglycerine (Tridil).
Atenolol (Tenormin).
Dobutamine (Dobutrex).
Norepinephrine (Levophed).
The Correct Answer is D
Norepinephrine is a vasopressor medication commonly used in the management of septic shock. It acts as a potent vasoconstrictor to increase systemic vascular resistance and improve blood pressure. By constricting blood vessels, norepinephrine helps restore tissue perfusion and improve organ function.
A. Nitroglycerine (Tridil) in (option A) is incorrect because: Nitroglycerine is a vasodilator and would further lower blood pressure. It is not suitable for a patient with septic shock who already has low blood pressure.
B. Atenolol (Tenormin) in (option B) is incorrect because: Atenolol is a beta-blocker and would further decrease heart rate and blood pressure. It is not appropriate for a patient in septic shock who requires intervention to increase blood pressure.
C. Dobutamine (Dobutrex) in (option C) is incorrect because: Dobutamine is an inotropic medication used to increase cardiac output. While it can be helpful in certain types of shock, such as cardiogenic shock, it is not the first-line choice for septic shock when there is inadequate blood pressure response.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
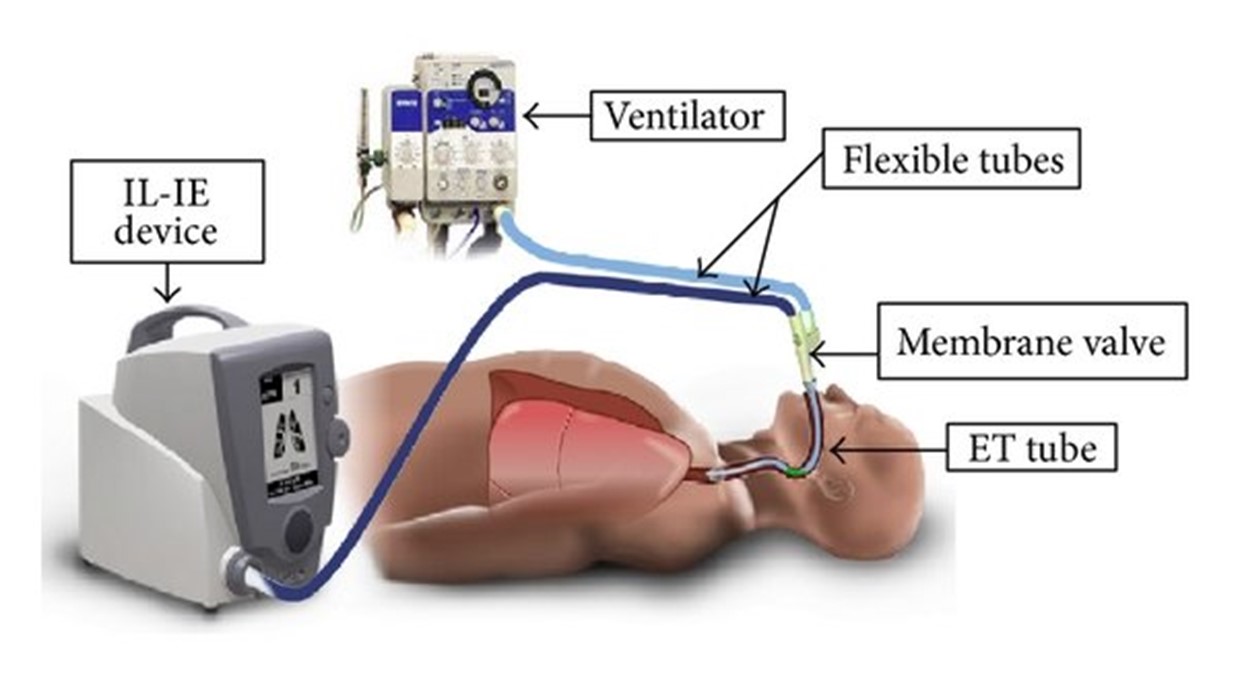
In a patient receiving mechanical ventilation, a high respiratory rate can indicate increased work of breathing and potential airway obstruction. COPD patients, in particular, may have excessive mucus production and airway inflammation, leading to mucus plugging and compromised airway clearance. Suctioning may be necessary to remove excessive secretions and maintain a patent airway.
A. The pulse oximeter shows a SpO2 of 90% in (option A) is incorrect because While a SpO2 of 90% is suboptimal and may require intervention, it does not specifically indicate the need for suctioning. Other interventions, such as adjusting oxygen delivery or ventilation settings, may be more appropriate.
B. The patient has not been suctioned for the last 6 hours in (option B) is incorrect because The duration since the last suctioning episode alone does not necessarily indicate the need for suctioning. The need for suctioning should be based on the patient's clinical presentation, such as signs of airway obstruction or excessive secretions.
D. The lungs have occasional audible expiratory wheezes in (option D) which is incorrect because Occasional audible expiratory wheezes may be common in patients with COPD and may not specifically indicate the need for suctioning. Wheezing is more commonly associated with narrowing of the airways, and suctioning is typically performed to clear secretions or maintain airway patency.
C. Therefore, in a COPD patient receiving mechanical ventilation, a high respiratory rate (C) is the assessment information that would indicate the need for suctioning to help remove excessive secretions and ensure a patent airway
Correct Answer is C
Explanation
The sepsis resuscitation bundle typically includes the administration of intravenous fluids to restore adequate perfusion and address hypovolemia. The initial fluid of choice is often the crystalloid solution, such as Lactated Ringers (LR), and the recommended initial fluid bolus is 30 ml/kg. This intervention aims to optimize intravascular volume and improve tissue perfusion.
A. Cooling baths in (option A) is incorrect because they may be used in the management of hyperthermia or fever, but they are not specific interventions in the sepsis resuscitation bundle.
B. Blood transfusion in (option B) is incorrect it may be necessary in certain cases of sepsis, such as severe anemia or hypovolemia, but it is not a routine intervention in the sepsis resuscitation bundle based solely on the provided information.
D. NPO status (nothing by mouth) in (option D) is incorrect because it is not a specific intervention in the sepsis resuscitation bundle. It may be indicated in certain cases, such as when surgery is required or if there is a risk of aspiration, but it does not directly address the sepsis-related variables mentioned.
It is important to note that the specific management of sepsis may vary based on the patient's individual condition, clinical presentation, and healthcare provider's orders.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
