The emergency department nurse reviews the medical record of a 41-year-old male patient with hemorrhagic shock, which contains the following information.
Physical Assessment Findings Pulse 140 beats/min and thready
Diagnostic Findings ABG respiratory acidosis
Blood pressure 60/40 mm Hg Respirations 40/min and shallow
Lactate level 7 mmol/L
All of these provider prescriptions are ordered for the patient. Which does the nurse carry out first?
Give Plasmanate 1 unit now.
Prepare for endotracheal intubation.
Give normal saline solution 250 mL/hr.
Type and crossmatch for 4 units of packed red blood cells (PRBCs).
The Correct Answer is C
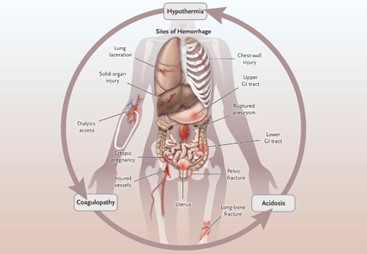
Hemorrhagic shock is characterized by severe blood loss, leading to inadequate tissue perfusion and hypovolemia. The primary goal in the initial management of hemorrhagic shock is to restore intravascular volume and improve tissue perfusion. Administering intravenous fluids, such as normal saline solution, is a critical intervention to address hypovolemia and improve blood pressure.
A. Give Plasmanate 1 unit now in (option A) is incorrect because: Plasmanate is a plasma-derived product used to replace coagulation factors. While it may be necessary to address coagulation abnormalities, administering intravenous fluids to restore volume takes priority over specific blood products.
B. Prepare for endotracheal intubation in (option B) is incorrect because Endotracheal intubation may be required in cases of impending respiratory failure or compromised airway, but it should not be the first action in addressing hypovolemic shock.
D. Type and crossmatch for 4 units of packed red blood cells (PRBCs) in (option D) is incorrect because transferring packed red blood cells is an important intervention to address blood loss and improve oxygen-carrying capacity. However, before administering blood products, it is crucial to stabilize the patient's hemodynamics through fluid resuscitation.
Therefore, in a patient with hemorrhagic shock, the nurse's first priority among the given options is to give normal saline solution of 250 mL/hr to restore intravascular volume and improve tissue perfusion.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Mean arterial pressure (MAP) is a measure of the average pressure within the arteries during one cardiac cycle. It represents the perfusion pressure that drives blood flow to organs and tissues. In the context of shock, a MAP of 50 mm Hg is considered low and indicates inadequate tissue perfusion.
To improve tissue perfusion and restore blood pressure, the nurse would anticipate administering large volumes of intravenous fluids, such as Lactated Ringers (LR). Fluid resuscitation aims to increase intravascular volume and improve cardiac output, ultimately leading to improved tissue perfusion.
B. Cardiac Output (CO) is 4 L/min in (option A) is incorrect because Cardiac output represents the volume of blood pumped by the heart per minute. While a low cardiac output may require intervention, it does not specifically indicate the need for large volumes of fluid administration.
C. Stroke volume is 70 ml/beat in (option C) is incorrect because Stroke volume refers to the volume of blood ejected by the heart with each contraction. While stroke volume can be an important determinant of cardiac output, it alone does not indicate the need for large fluid volumes.
D. The heart rate is 80 bpm in (option D) is incorrect because: Heart rate is the number of heartbeats per minute. While the heart rate can impact cardiac output, it does not provide direct information about fluid resuscitation needs.
Correct Answer is A
Explanation
The increased respiratory rate and pulse rate can be indicators of physiological changes or potential complications in the patient's condition. These changes may suggest alterations in tissue perfusion or other underlying issues that require further assessment.
Assessing the patient's tissue perfusion includes evaluating additional vital signs, such as blood pressure, oxygen saturation, and capillary refill time. Assessing skin color, temperature, and moisture, as well as peripheral pulses, can also provide important information regarding tissue perfusion.
B. Pain medication (option B) is incorrect because the increased respiratory and pulse rates could also indicate other factors that require assessment before administering pain medication.
C. Documenting the findings in the patient's chart (option C) is incorrect because it should not be the primary action at this point. Assessing the patient's condition and determining appropriate interventions take priority.
D. Increasing the rate of the patient's IV infusion (option D) is incorrect because may not be the most appropriate action without further assessment. The patient's increased respiratory and pulse rates may not necessarily be related to hydration status, and it is important to assess the patient comprehensively before making changes to the IV infusion rate.
Therefore, the best action by the nurse in this situation is to further assess the patient's tissue perfusion to gather more information and determine the appropriate course of action.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
