A 31-year-old male patient with burn injuries is admitted to the burn unit. Which priority does the nurse anticipate within the first 24 hours?
Sterile dressing changes
Emotional support
Fluid resuscitation
Range-of-motion exercises
The Correct Answer is C
In the initial 24 hours after burn injury, fluid resuscitation is a critical priority in the management of burn patients. Burn injuries can lead to significant fluid loss, both locally at the burn site and systemically due to increased capillary permeability. Fluid resuscitation aims to restore and maintain adequate intravascular volume, ensuring sufficient tissue perfusion and organ function.
The Parkland Formula is commonly used to guide fluid resuscitation in burn patients. It involves calculating the total volume of fluid needed in the first 24 hours, with a portion given in the initial hours after injury and the remainder given over the remaining hours.
A. Sterile dressing changes (option A) are incorrect because they are important in wound care management for burn patients to prevent infection. However, fluid resuscitation takes precedence within the first 24 hours.
B. Emotional support (option B) is incorrect because it is an essential aspect of burn care, as burn injuries can have a significant psychological impact. While emotional support is crucial for the patient's overall well-being, it may not be the highest priority within the first 24 hours compared to addressing the physiological needs of fluid resuscitation.
D. Range-of-motion exercises (option D) are incorrect because they are important for preventing contractures and maintaining joint mobility in burn patients. However, they are typically initiated after the initial fluid resuscitation phase and wound stabilization.
Therefore, the priority the nurse anticipates within the first 24 hours for a 31-year-old male patient with burn injuries is fluid resuscitation.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Assessing tissue perfusion is crucial in evaluating the adequacy of oxygen and nutrient delivery to the body's tissues. While multiple factors contribute to tissue perfusion, the options provided in choice B are key indicators:
Level of consciousness: Altered mental status or changes in the patient's level of consciousness can be a sign of impaired cerebral perfusion, which reflects overall tissue perfusion.
Urine output: Monitoring urine output provides information about renal perfusion and kidney function. Decreased urine output can be indicative of inadequate tissue perfusion.
Lactate level: Lactate is a by-product of anaerobic metabolism that accumulates when there is insufficient oxygen delivery to tissues. Elevated lactate levels indicate tissue hypoperfusion and cellular oxygen debt.
A. Pupil response, pulse pressure, and urine output in (option A) are incorrect because While pupil response and pulse pressure may provide some information about perfusion, they do not encompass a comprehensive assessment of tissue perfusion. Additionally, assessing urine output is important, but it alone may not provide a complete picture of tissue perfusion status.
C. Blood pressure, pulse, and respirations in (option C) are incorrect because Blood pressure, pulse, and respirations are important vital signs to monitor, but they do not solely indicate tissue perfusion. Hypotension, for example, can be a late sign of inadequate tissue perfusion.
D. Breath sounds, heart rate, and pupil response in (option D) are incorrect because: Although breath sounds and heart rate can be affected by changes in tissue perfusion, they are not specific or comprehensive indicators of tissue perfusion status. Pupil response alone does not provide a complete assessment of tissue perfusion.
Therefore, the most accurate assessment of tissue perfusion in a patient in shock involves evaluating the level of consciousness, urine output, and lactate levels.
Correct Answer is D
Explanation
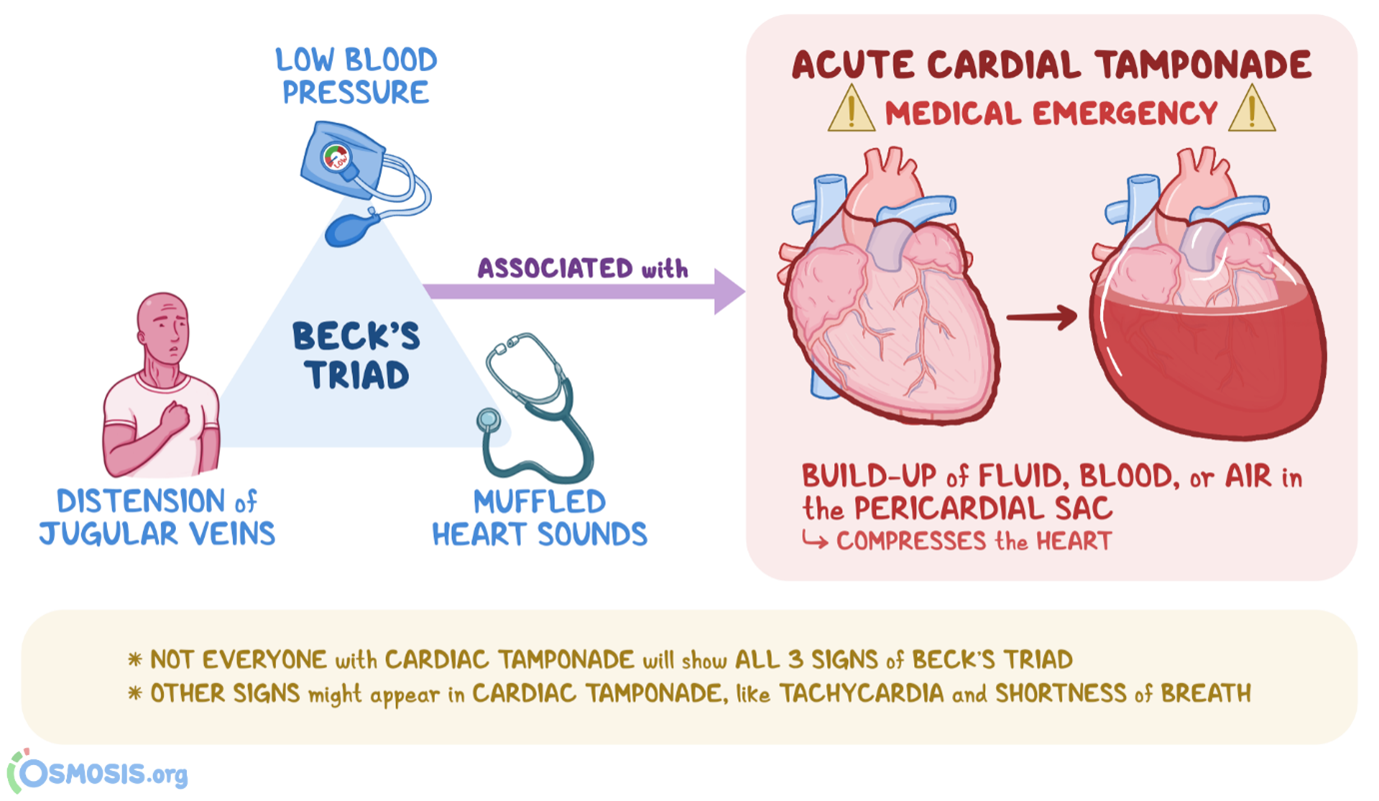
Beck's triad consists of three classic clinical manifestations that are suggestive of cardiac tamponade, which is the compression of the heart by accumulated fluid or blood within the pericardial sac. The three components of Beck's triad include:
A. Muffled heart tones in (option A) are incorrect because Cardiac tamponade can dampen or muffle heart sounds due to the presence of fluid or blood around the heart, which can impair sound transmission.
B. Marked hypotension in (option B) is incorrect because Cardiac tamponade can cause decreased cardiac output, leading to hypotension, which is characterized by low blood pressure.
C. Distended jugular veins in (option C) is incorrect because Elevated venous pressure resulting from impaired filling and elevated right-sided heart pressures can lead to jugular vein distension, which is commonly seen in cardiac tamponade.
However, widening pulse pressure (the difference between systolic and diastolic blood pressure) is not typically part of Beck's triad. Widening pulse pressure is associated with her conditions such as aortic regurgitation, hyperthyroidism, or conditions involving increased stroke volume, rather than cardiac tamponade specifically.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
