A 32-year-old male patient sustains 78% TBSA burn and is currently admitted to the burn unit. Which sequential order would the nurse arrange the events involved in burn shock following a patient's exposure to burns?
Decreased blood volume
Increased Increased vascular permeability
peripheral resistance
Development of edema
The Correct Answer is A,B,D,C
A. Decreased blood volume: Burn injuries can lead to fluid loss, primarily through damaged skin. This fluid loss causes a decrease in blood volume, leading to hypovolemia. Hypovolemia contributes to decreased cardiac output and tissue perfusion.
B. Increased vascular permeability: Burn injuries cause an inflammatory response, leading to increased vascular permeability. This increased permeability allows fluid, electrolytes, and proteins to leak from the intravascular space into the interstitial space.
C. Development of edema: The increased vascular permeability and fluid leakage lead to the development of edema. Edema occurs as fluid accumulates in the interstitial spaces, further contributing to tissue swelling and compromised perfusion.
D. Increased peripheral resistance: In response to decreased blood volume and tissue hypoperfusion, the body activates compensatory mechanisms to maintain blood pressure and tissue perfusion. One of these mechanisms is increased peripheral resistance, which occurs as blood vessels constrict to maintain blood pressure. Increased peripheral resistance helps redirect blood flow to vital organs but also contributes to increased workload on the heart.
Therefore, the correct sequential order of events involved in burn shock following a patient's exposure to burns is:
A. Decreased blood volume B. Increased vascular permeability D. Development of edema C. Increased peripheral resistance
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Arterial pressure monitoring involves the insertion of an arterial catheter, typically in the radial artery, to directly measure blood pressure. Complications can arise from this invasive procedure, and one potential complication is inadequate blood flow to the hand, leading to numbness or ischemia.
A. The Allen's test is positive in (option A) is incorrect because The Allen's test is performed before arterial catheter insertion to assess the collateral circulation of the hand. A positive Allen test indicates adequate collateral circulation, which is desirable before performing the procedure. However, it does not directly indicate a complication during or after arterial pressure monitoring.
B. The mean arterial pressure (MAP) is 90 mm Hg in (option B) is incorrect because The mean arterial pressure (MAP) represents the average pressure in the arterial system during one cardiac cycle. While changes in MAP can be significant for patient management, it does not specifically indicate a complication of arterial pressure monitoring.
C. The dicrotic notch visible in the waveform in (option C) is incorrect because The dicrotic notch represents the closure of the aortic valve and is a normal finding in arterial waveforms. Its presence does not indicate a complication.
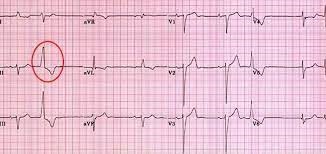
Correct Answer is A
Explanation
Premature ventricular contractions (PVCs) are abnormal heart rhythms originating from the ventricles. They can be triggered by various factors, including irritation or stimulation of the airway during suctioning.
In this situation, the priority is to ensure adequate oxygenation and ventilation for the patient. Stopping the suctioning procedure and providing ventilatory support with 100% oxygen helps maintain oxygen levels and minimizes further cardiac dysrhythmias.
B. Check the patient's potassium level in (option B) is incorrect because While electrolyte imbalances, including low potassium levels (hypokalemia), can contribute to cardiac dysrhythmias, checking the potassium level is not the immediate priority when PVCs occur during suctioning.
C. Give prescribed PRN antidysrhythmic medications in (option C) is incorrect because: Administering antidysrhythmic medications without further assessment or evaluation may not be appropriate in this situation.
D. Decrease the suction pressure to 80 mm Hg in (option D) is incorrect because: While adjusting suction pressure may help prevent further irritation, it is not the initial priority when PVCs are present during suctioning.
E. Documenting the dysrhythmia in the patient's chart in (option E) is incorrect because: Documentation is important but should not be the initial action when a patient experiences PVCs during suctioning. Patient safety and immediate intervention take precedence.
Therefore, when PVCs occur during suctioning, the nurse should stop the procedure, provide ventilatory support with 100% oxygen, and assess the patient's response to intervention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
