The ICU charge nurse will evaluate that teaching about hemodynamic monitoring for a new staff nurse has been effective when the new nurse does which of the following?
Position the limb with the catheter insertion site at the level of the transducer.
Positions the transducer level with the phlebostatic axis.
Ensures that the patient is lying with the head of the bed flat for all readings.
Balances and calibrates the hemodynamic monitoring equipment every hour.
The Correct Answer is B
Positioning the transducer level with the phlebostatic axis is a crucial step in accurate hemodynamic monitoring. The phlebostatic axis is an imaginary reference point located at the fourth intercostal space, mid-anterior/posterior chest. Placing the transducer at this level ensures that the pressure measurements obtained are reflective of the patient's true hemodynamic status.
A. Positioning the limb with the catheter insertion site at the level of the transducer in (option A) is incorrect because: While it is important to position the limb appropriately to avoid kinks or occlusions in the catheter tubing, this is not directly related to the accurate measurement of hemodynamic parameters.
C. Ensuring that the patient is lying with the head of the bed flat for all readings in (option C) is incorrect because The position of the patient's head does not directly impact the accuracy of hemodynamic monitoring unless it specifically relates to changes in preload or intracranial pressure monitoring.
D. Balancing and calibrating the hemodynamic monitoring equipment every hour in (option D) is incorrect because: While it is important to ensure that the monitoring equipment is calibrated and functioning properly, doing so every hour may not be necessary. Calibration frequency may vary based on institutional policies and patient stability.
Therefore, the correct action that demonstrates effective teaching about hemodynamic monitoring is positioning the transducer level with the phlebostatic axis.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Tachypnoea, which refers to an increased respiratory rate, is an early symptom of hypovolemic shock. It is the body's compensatory response to inadequate tissue perfusion and decreased oxygen delivery. The increased respiratory rate is an attempt to improve oxygenation and maintain vital organ function.
B. Heart blocks in (option B) are incorrect because Heart blocks refer to disruptions in the electrical conduction system of the heart and are not specific to hypovolemic shock.
C. Vomiting in (option C) is incorrect because: Vomiting may occur in various conditions, including shock, but it is not exclusive to hypovolemic shock and can be present in other forms of shock or illnesses.
D. Bradycardia in (option D) is incorrect because Bradycardia, or a slow heart rate, is not typically an early symptom of hypovolemic shock. Instead, tachycardia (rapid heart rate) is more commonly observed as a compensatory response to maintain cardiac output.
E. Hypotension in (option E) is incorrect because Hypotension, or low blood pressure, can occur in hypovolemic shock but is generally considered a later-stage symptom. In the early stages, compensatory mechanisms may help maintain blood pressure, so hypotension may not be present initially.
F. Bradypnea in (option F) is incorrect because: Bradypnea refers to a slow respiratory rate, which is not typically an early symptom of hypovolemic shock. Tachypnoea, as mentioned earlier, is the more common early respiratory symptom.
Correct Answer is D
Explanation
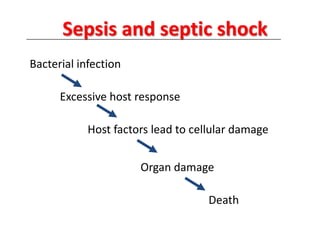
Septic shock is a life-threatening condition characterized by severe infection, systemic inflammation, and inadequate tissue perfusion. Hypotension, as indicated by a low blood pressure reading, is a significant concern in septic shock. It reflects inadequate perfusion to vital organs and tissues, leading to potential organ dysfunction and damage.
While all the assessment data provided may be important and require attention, the low blood pressure (BP) reading indicates impaired systemic perfusion and can contribute to end-organ damage. The nurse should prioritize interventions aimed at improving perfusion and stabilizing the patient's blood pressure.
A. Arterial oxygen saturation is 90% in (option A) is incorrect because While an arterial oxygen saturation of 90% is below the desired range, it is not as immediately life-threatening as low blood pressure. Oxygen therapy and interventions to improve oxygenation should still be initiated, but addressing hypotension takes priority.
B. Urine output of 15 ml for 2 hours in (option B) is incorrect because Decreased urine output is a concerning sign, as it may indicate impaired renal perfusion. However, the immediate concern in septic shock is addressing the low blood pressure to improve overall perfusion, including renal perfusion.
C. Apical pulse 110 beats/min in (option C) is incorrect because: Tachycardia is a common finding in septic shock and represents the body's compensatory response to maintain cardiac output. While it requires monitoring and consideration, low blood pressure is a more significant concern.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
