The surgical ICU nurse is caring for postoperative clients at risk for hypovolemic shock. Which condition represents an early symptom of shock?
Tachypnoea
Heart blocks
Vomiting
Bradycardia
Hypotension
The Correct Answer is A
Tachypnoea, which refers to an increased respiratory rate, is an early symptom of hypovolemic shock. It is the body's compensatory response to inadequate tissue perfusion and decreased oxygen delivery. The increased respiratory rate is an attempt to improve oxygenation and maintain vital organ function.
B. Heart blocks in (option B) are incorrect because Heart blocks refer to disruptions in the electrical conduction system of the heart and are not specific to hypovolemic shock.
C. Vomiting in (option C) is incorrect because: Vomiting may occur in various conditions, including shock, but it is not exclusive to hypovolemic shock and can be present in other forms of shock or illnesses.
D. Bradycardia in (option D) is incorrect because Bradycardia, or a slow heart rate, is not typically an early symptom of hypovolemic shock. Instead, tachycardia (rapid heart rate) is more commonly observed as a compensatory response to maintain cardiac output.
E. Hypotension in (option E) is incorrect because Hypotension, or low blood pressure, can occur in hypovolemic shock but is generally considered a later-stage symptom. In the early stages, compensatory mechanisms may help maintain blood pressure, so hypotension may not be present initially.
F. Bradypnea in (option F) is incorrect because: Bradypnea refers to a slow respiratory rate, which is not typically an early symptom of hypovolemic shock. Tachypnoea, as mentioned earlier, is the more common early respiratory symptom.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
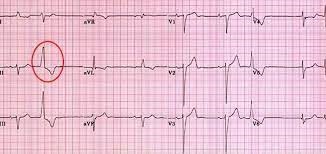
Correct Answer is C
Explanation
This method, known as the 6-second method, involves counting the number of QRS complexes in a 6-second interval on the electrocardiogram (ECG) strip and then multiplying that number by 10 to calculate the heart rate per minute. The advantage of this method is that it provides a relatively quick estimate of the heart rate.
A. Printing a 1-minute ECG strip and counting the number of QRS complexes in (option A) is incorrect because it can be time-consuming and may not be practical in situations where a quick estimate is needed.
B. Calculating the number of small squares between one QRS complex and the next and dividing into 1500 in (option B) is incorrect because it is a method used to calculate heart rate, known as the "1500 method," but it is not as quick as the 6-second method and requires more time and measurement precision.
D. Counting the number of large squares in the R-R interval and dividing by 300 is another method used to calculate heart rate, known as the "300 method," but it is also less quick and less accurate for assessing heart rate in patients with regular rhythms.
It's important to note that if the heart rhythm is irregular, these methods may not provide an accurate estimate of the heart rate, and a longer monitoring period or a different approach may be necessary.
Correct Answer is A
Explanation
Premature ventricular contractions (PVCs) are abnormal heart rhythms originating from the ventricles. They can be triggered by various factors, including irritation or stimulation of the airway during suctioning.
In this situation, the priority is to ensure adequate oxygenation and ventilation for the patient. Stopping the suctioning procedure and providing ventilatory support with 100% oxygen helps maintain oxygen levels and minimizes further cardiac dysrhythmias.
B. Check the patient's potassium level in (option B) is incorrect because While electrolyte imbalances, including low potassium levels (hypokalemia), can contribute to cardiac dysrhythmias, checking the potassium level is not the immediate priority when PVCs occur during suctioning.
C. Give prescribed PRN antidysrhythmic medications in (option C) is incorrect because: Administering antidysrhythmic medications without further assessment or evaluation may not be appropriate in this situation.
D. Decrease the suction pressure to 80 mm Hg in (option D) is incorrect because: While adjusting suction pressure may help prevent further irritation, it is not the initial priority when PVCs are present during suctioning.
E. Documenting the dysrhythmia in the patient's chart in (option E) is incorrect because: Documentation is important but should not be the initial action when a patient experiences PVCs during suctioning. Patient safety and immediate intervention take precedence.
Therefore, when PVCs occur during suctioning, the nurse should stop the procedure, provide ventilatory support with 100% oxygen, and assess the patient's response to intervention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
