Which of the following would the nurse include in the plan of care for a newborn receiving phototherapy? Select one:
Applying Vaseline or lotion to newborn to maximize light absorption.
Reducing the amount of fluid intake to 8 ounces daily.
Keeping the newborn in the supine position.
Feeding every 3 hours to maximize intake of fluids and output.
The Correct Answer is D
Choice A Reason: Applying Vaseline or lotion to newborn to maximize light absorption. This is an incorrect answer that indicates a contraindicated and harmful intervention that can interfere with phototherapy. Applying Vaseline or lotion to newborn can create a barrier or a reflective surface that can reduce the exposure and penetration of light to the skin, which can decrease the efficacy of phototherapy. Applying Vaseline or lotion to newborn can also cause skin irritation, infection, or burns, as it can trap heat and moisture under the light source.
Choice B Reason: Reducing the amount of fluid intake to 8 ounces daily. This is an incorrect answer that suggests a detrimental and dangerous intervention that can impair phototherapy. Reducing the amount of fluid intake to 8 ounces daily can cause dehydration, hypoglycemia, or electrolyte imbalance in newborns, which can worsen jaundice and increase the risk of complications such as kernicterus (brain damage due to high bilirubin levels). Reducing the amount of fluid intake to 8 ounces daily can also decrease the excretion of bilirubin through urine or stool, which can counteract the effect of phototherapy.
Choice C Reason: Keeping the newborn in the supine position. This is an incorrect answer that implies an incomplete and inadequate intervention that can limit phototherapy. Keeping the newborn in the supine position is a nursing action that involves placing the newborn on their back, which can expose their anterior body surface to light.
However, keeping the newborn in the supine position alone is not sufficient for phototherapy, as it does not expose their posterior body surface to light. The nurse should also reposition the newborn frequently to expose different body parts to light, such as their sides or abdomen.
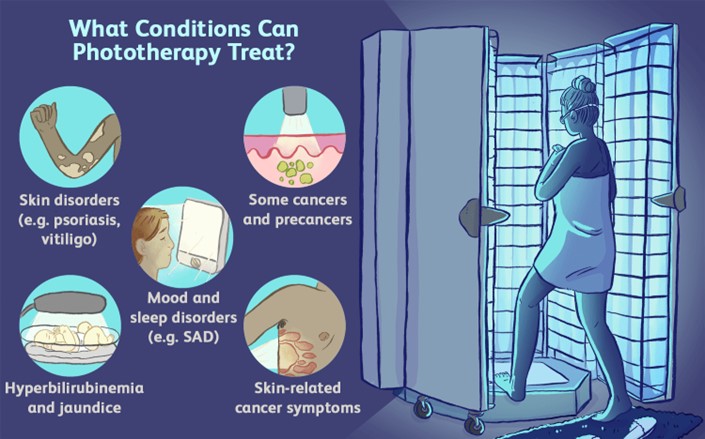
Choice D Reason: Feeding every 3 hours to maximize intake of fluids and output. This is because feeding every 3 hours is a nursing intervention that can enhance the effectiveness and safety of phototherapy, which is a treatment that uses blue or white light to reduce the level of bilirubin in the blood. Bilirubin is a yellow pigment that is produced when red blood cells are broken down, which can cause jaundice (yellowish discoloration of the skin and mucous membranes) if it accumulates in excess. Phototherapy works by converting bilirubin into a water-soluble form that can be excreted through urine or stool. Feeding every 3 hours can increase the intake of fluids and calories, which can promote hydration, nutrition, and elimination of bilirubin.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: About 1 of every 5 women will experience abuse in her lifetime is a statistic that shows the prevalence of domestic violence, but it does not address the question of what the nurse should emphasize to the group of women.
Choice B Reason: When women go back to the situation after the abuser has calmed down, things will be beter is a false statement that reflects the cycle of abuse, where the abuser may apologize and promise to change after a violent episode, but then repeat the same behavior later. This does not help the women understand their situation or seek help.
Choice C Reason: The victimized woman can easily leave the situation is a false statement that ignores the many barriers and challenges that women face when trying to escape from domestic violence, such as fear, isolation, financial dependence, lack of support, legal issues, and threats from the abuser. This does not empower the women or provide them with realistic options.
Choice D Reason: The violence will not stop or decrease if the woman becomes pregnant is a true statement that highlights the danger of staying in an abusive relationship during pregnancy. Domestic violence can increase the risk of miscarriage, preterm birth, low birth weight, placental abruption, fetal injury, and maternal death. This may motivate the women to seek safety and protection for themselves and their unborn children.
Correct Answer is D
Explanation
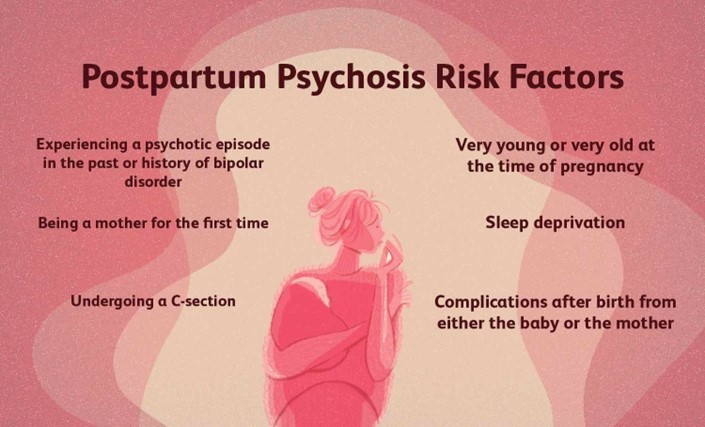
Choice A Reason: Maintain the client on strict bedrest. This is an inappropriate action that may worsen the client's condition and increase her isolation and depression. Postpartum psychosis requires prompt psychiatric treatment with medication and psychotherapy, not bedrest.
Choice B Reason: Carefully monitor intake and output. This is an irrelevant action that has no direct relation to postpartum psychosis or its management. Monitoring intake and output may be indicated for other postpartum complications such as hemorrhage, infection, or preeclampsia.
Choice C Reason: Restrict visitation of the client's partner. This is an unnecessary action that may deprive the client of social support and emotional comfort. The partner may be an important source of help and information for the client and the health care team. The partner should be involved in the client's care and education, unless there are signs of abuse or violence.
Choice D Reason: Closely supervise all infant care and interaction. This is because postpartum psychosis is a severe mental disorder that occurs in some women after childbirth, which can cause delusions, hallucinations, paranoia, mood swings, confusion, and suicidal or homicidal thoughts. Postpartum psychosis can pose a danger to both the mother and the infant, as the mother may harm herself or the infant due to distorted perceptions or impulses. The nurse should closely supervise all infant care and interaction to ensure safety and prevent injury.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
