A client with insulin-dependent type 2 diabetes and an HbA1c of 6.0% is planning to become pregnant soon. What anticipatory teaching should the nurse provide this client?
Select one:
Insulin needs decrease in the first trimester, but increase in the second trimester as the woman's body becomes more insulin-resistant.
Vascular disease that always accompanies diabetes slows fetal growth.
The risk of ketoacidosis decreases during the length of the pregnancy.
The baby is likely to have a congenital abnormality because of the uncontrolled diabetes.
The Correct Answer is A
Choice A Reason: Insulin needs decrease in the first trimester, but increase in the second trimester as the woman's body becomes more insulin-resistant. This is because this statement describes the typical patern of insulin requirements during pregnancy for women with pre-existing diabetes. Insulin needs decrease in the first trimester due to increased insulin production by the pancreas, increased insulin sensitivity by the tissues, and increased risk of hypoglycemia due to nausea and vomiting. Insulin needs increase in the second trimester due to increased levels of placental hormones such as human placental lactogen (hPL), which antagonize insulin action and cause insulin resistance.
Choice B Reason: Vascular disease that always accompanies diabetes slows fetal growth. This is an incorrect answer that makes a false and exaggerated claim about diabetes and fetal growth. Vascular disease does not always accompany diabetes, but it can be a complication of long-term or poorly controlled diabetes that affects blood vessels and circulation. Vascular disease can affect fetal growth by reducing placental perfusion and oxygen delivery, but it is not the only factor that influences fetal growth. Other factors include maternal nutrition, genetics, infections, or anomalies.
Choice C Reason: The risk of ketoacidosis decreases during the length of the pregnancy. This is an incorrect answer that contradicts the evidence and guidelines on diabetes and ketoacidosis during pregnancy. Ketoacidosis is a metabolic emergency where high levels of ketones accumulate in the blood due to insufficient insulin or excessive glucose utilization, which causes acidosis, dehydration, electrolyte imbalance, and coma. Ketoacidosis can occur in women with diabetes during pregnancy due to infection, stress, starvation, or inadequate insulin therapy. The risk of ketoacidosis does not decrease during the length of the pregnancy, but rather increases in the second and third trimesters due to increased insulin resistance and glucose production.
Choice D Reason: The baby is likely to have a congenital abnormality because of the uncontrolled diabetes. This is an incorrect answer that implies a negative and deterministic outcome for the baby. Congenital abnormalities are structural or functional defects that are present at birth, which can affect various organs or systems in the baby.
Congenital abnormalities can be caused by genetic or environmental factors, or a combination of both. Diabetes can increase the risk of congenital abnormalities, especially if the blood glucose levels are high during the first trimester, when organogenesis occurs. However, the risk of congenital abnormalities is not inevitable or predictable, and it can be reduced by maintaining good glycemic control before and during pregnancy.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: About 1 of every 5 women will experience abuse in her lifetime is a statistic that shows the prevalence of domestic violence, but it does not address the question of what the nurse should emphasize to the group of women.
Choice B Reason: When women go back to the situation after the abuser has calmed down, things will be beter is a false statement that reflects the cycle of abuse, where the abuser may apologize and promise to change after a violent episode, but then repeat the same behavior later. This does not help the women understand their situation or seek help.
Choice C Reason: The victimized woman can easily leave the situation is a false statement that ignores the many barriers and challenges that women face when trying to escape from domestic violence, such as fear, isolation, financial dependence, lack of support, legal issues, and threats from the abuser. This does not empower the women or provide them with realistic options.
Choice D Reason: The violence will not stop or decrease if the woman becomes pregnant is a true statement that highlights the danger of staying in an abusive relationship during pregnancy. Domestic violence can increase the risk of miscarriage, preterm birth, low birth weight, placental abruption, fetal injury, and maternal death. This may motivate the women to seek safety and protection for themselves and their unborn children.
Correct Answer is A
Explanation
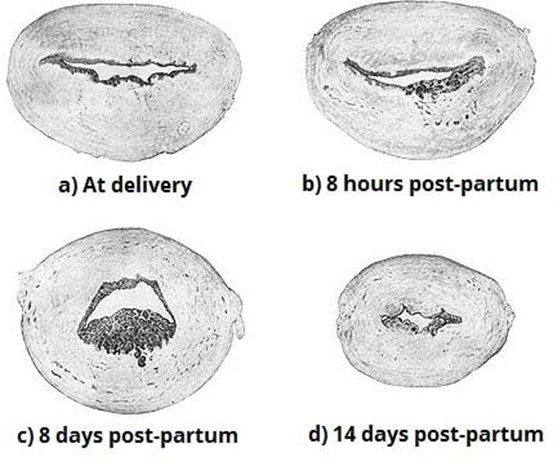
Choice A Reason: Inspecting the placenta after delivery for intactness. This is because inspecting the placenta after delivery for intactness is a nursing intervention that can prevent late postpartum hemorrhage, which is excessive bleeding from the uterus or genital tract that occurs more than 24 hours but less than 12 weeks after delivery. Late postpartum hemorrhage can be caused by retained placental fragments, subinvolution of the uterus, infection, or coagulation disorders. Inspecting the placenta after delivery for intactness can help identify and remove any retained placental fragments that may interfere with uterine contraction and involution, which are essential for hemostasis.
Choice B Reason: Manually removing the placenta at delivery. This is an incorrect answer that indicates an inappropriate and risky intervention that can cause late postpartum hemorrhage. Manually removing the placenta at delivery is a procedure that involves inserting a hand into the uterus and detaching the placenta from the uterine wall. Manually removing the placenta at delivery is indicated only for a retained or adherent placenta that does not separate spontaneously or with gentle traction within 30 minutes after delivery. Manually removing the placenta at delivery can cause trauma, infection, or incomplete removal of the placenta, which can increase the risk of late postpartum hemorrhage.
Choice C Reason: Administering broad-spectrum antibiotics prophylactically. This is an incorrect answer that suggests an unnecessary and ineffective intervention that can prevent late postpartum hemorrhage. Administering broad- spectrum antibiotics prophylactically is a pharmacological intervention that involves giving antibiotics to prevent or treat infection. Administering broad-spectrum antibiotics prophylactically is indicated for women with risk factors or signs of infection during or after delivery, such as prolonged rupture of membranes, chorioamnionitis, fever, or foul- smelling lochia. Administering broad-spectrum antibiotics prophylactically may reduce the risk of infection-related late postpartum hemorrhage, but it does not address other causes of late postpartum hemorrhage such as retained placental fragments or subinvolution of the uterus.
Choice D Reason: Applying traction on the umbilical cord to speed up separation of the placenta. This is an incorrect answer that refers to a different intervention that can prevent early postpartum hemorrhage, not late postpartum hemorrhage. Applying traction on the umbilical cord to speed up separation of the placenta is a technique that involves pulling on the umbilical cord while applying counter pressure on the uterus to facilitate placental expulsion. Applying traction on the umbilical cord to speed up separation of the placenta is indicated for active management of the third stage of labor, which can prevent early postpartum hemorrhage, which is excessive bleeding from the uterus or genital tract that occurs within 24 hours after delivery. Early postpartum hemorrhage can be caused by uterine atony, retained placenta, lacerations, or coagulation disorders.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
