Which of the following would be essential to implement to prevent late postpartum hemorrhage? Select one:
Inspecting the placenta after delivery for intactness.
Manually removing the placenta at delivery.
Administering broad-spectrum antibiotics prophylactically.
Applying traction on the umbilical cord to speed up separation of the placenta.
The Correct Answer is A
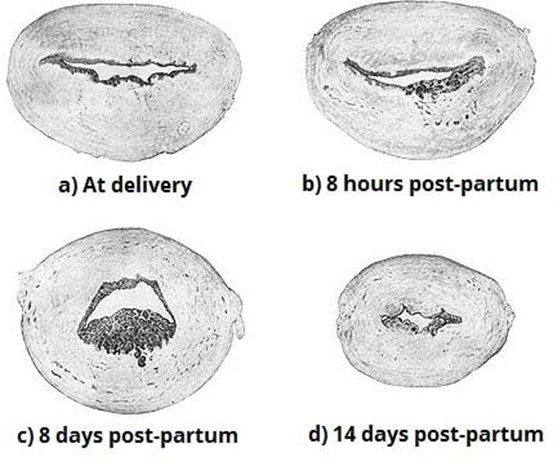
Choice A Reason: Inspecting the placenta after delivery for intactness. This is because inspecting the placenta after delivery for intactness is a nursing intervention that can prevent late postpartum hemorrhage, which is excessive bleeding from the uterus or genital tract that occurs more than 24 hours but less than 12 weeks after delivery. Late postpartum hemorrhage can be caused by retained placental fragments, subinvolution of the uterus, infection, or coagulation disorders. Inspecting the placenta after delivery for intactness can help identify and remove any retained placental fragments that may interfere with uterine contraction and involution, which are essential for hemostasis.
Choice B Reason: Manually removing the placenta at delivery. This is an incorrect answer that indicates an inappropriate and risky intervention that can cause late postpartum hemorrhage. Manually removing the placenta at delivery is a procedure that involves inserting a hand into the uterus and detaching the placenta from the uterine wall. Manually removing the placenta at delivery is indicated only for a retained or adherent placenta that does not separate spontaneously or with gentle traction within 30 minutes after delivery. Manually removing the placenta at delivery can cause trauma, infection, or incomplete removal of the placenta, which can increase the risk of late postpartum hemorrhage.
Choice C Reason: Administering broad-spectrum antibiotics prophylactically. This is an incorrect answer that suggests an unnecessary and ineffective intervention that can prevent late postpartum hemorrhage. Administering broad- spectrum antibiotics prophylactically is a pharmacological intervention that involves giving antibiotics to prevent or treat infection. Administering broad-spectrum antibiotics prophylactically is indicated for women with risk factors or signs of infection during or after delivery, such as prolonged rupture of membranes, chorioamnionitis, fever, or foul- smelling lochia. Administering broad-spectrum antibiotics prophylactically may reduce the risk of infection-related late postpartum hemorrhage, but it does not address other causes of late postpartum hemorrhage such as retained placental fragments or subinvolution of the uterus.
Choice D Reason: Applying traction on the umbilical cord to speed up separation of the placenta. This is an incorrect answer that refers to a different intervention that can prevent early postpartum hemorrhage, not late postpartum hemorrhage. Applying traction on the umbilical cord to speed up separation of the placenta is a technique that involves pulling on the umbilical cord while applying counter pressure on the uterus to facilitate placental expulsion. Applying traction on the umbilical cord to speed up separation of the placenta is indicated for active management of the third stage of labor, which can prevent early postpartum hemorrhage, which is excessive bleeding from the uterus or genital tract that occurs within 24 hours after delivery. Early postpartum hemorrhage can be caused by uterine atony, retained placenta, lacerations, or coagulation disorders.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: Enhance uterine contractions. This is an incorrect answer that contradicts the effect of narcotic analgesia on uterine activity. Narcotic analgesia can reduce uterine contractions by decreasing maternal catecholamine levels, which can prolong labor or increase bleeding.
Choice B Reason: Be used in place of preoperative sedation. This is an irrelevant answer that does not apply to this scenario. Preoperative sedation is a medication given before surgery to reduce anxiety, pain, or nausea. Narcotic analgesia can be used as a preoperative sedative, but it is not related to labor or delivery.
Choice C Reason: Result in neonatal respiratory depression. This is because narcotic analgesia can cross the placenta and affect the fetal central nervous system, which can cause decreased respiratory drive, apnea, bradycardia, or hypotonia in the newborn. The risk of neonatal respiratory depression is higher when narcotic analgesia is administered close to delivery, as there is less time for placental clearance or maternal metabolism.
Choice D Reason: Prevent the need for anesthesia with an episiotomy. This is an inaccurate answer that overestimates the effect of narcotic analgesia on perineal pain. Narcotic analgesia can provide some relief of labor pain, but it does not block pain sensation completely or locally. An episiotomy is a surgical incision made in the perineum to enlarge the vaginal opening during delivery, which requires local anesthesia or regional anesthesia (such as epidural or spinal). Narcotic analgesia does not prevent or replace anesthesia with an episiotomy.
Correct Answer is C
Explanation
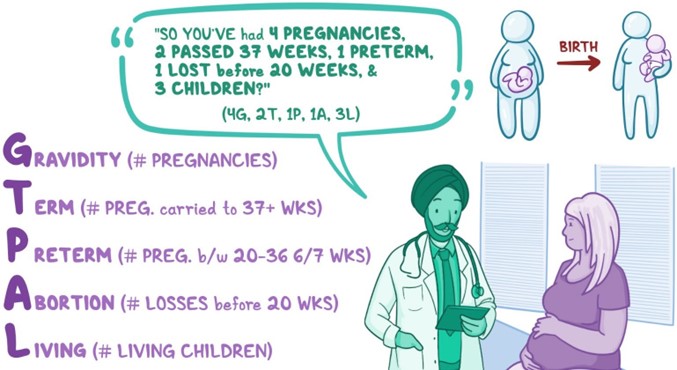
Choice A Reason: 3-2-1-0-2. This is an incorrect answer that underestimates the number of pregnancies and overestimates the number of preterm births. The client has had four pregnancies, not three. She has had one preterm birth, not two.
Choice B Reason: 4-1-1-1-3. This is an incorrect answer that overestimates the number of living children. The client has two living children, not three.
Choice C Reason 4-1-1-1-2. This is because the GTPAL method is a way of summarizing a woman's obstetric history using five numbers: G (gravida), T (term births), P (preterm births), A (abortions), and L (living children). Gravida is the number of pregnancies, regardless of outcome. Term births are deliveries after 37 weeks' gestation. Preterm births are deliveries between 20 and 37 weeks' gestation. Abortions are pregnancies that end before 20 weeks' gestation, either spontaneously or electively. Living children are the number of children who are alive at the time of assessment.
Choice D Reason: 4-1-2-0-3. This is an incorrect answer that overestimates the number of preterm births and living children, and underestimates the number of abortions. The client has had one preterm birth, not two. She has had one abortion, not zero. She has two living children, not three.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
