Before applying a cord clamp, the nurse assesses the umbilical cord for vessels. The nurse expects to find: Select one:
Two arteries, one vein.
Two veins, one artery.
Two veins, two arteries.
One artery, one vein.
The Correct Answer is A
Choice A Reason: Two arteries, one vein. This is because two arteries and one vein are the normal components of the umbilical cord, which is a structure that connects the fetus to the placenta and provides blood circulation between them. The umbilical cord carries oxygenated blood from the placenta to the fetus through the umbilical vein, and deoxygenated blood from the fetus to the placenta through the umbilical arteries.
Choice B Reason: Two veins, one artery. This is an incorrect answer that indicates an abnormal anatomy of the umbilical cord, which is known as single umbilical artery (SUA). SUA is a condition where there is only one umbilical artery instead of two, which can reduce blood flow and oxygen delivery to the fetus. SUA can be associated with congenital anomalies or growth restriction in some cases.
Choice C Reason: Two veins, two arteries. This is an incorrect answer that indicates an abnormal anatomy of the umbilical cord, which is known as double umbilical vein (DUV). DUV is a condition where there are two umbilical veins instead of one, which can increase blood flow and oxygen delivery to the fetus. DUV can be associated with fetal overgrowth or polycythemia in some cases.
Choice D Reason: One artery, one vein. This is an incorrect answer that indicates an abnormal anatomy of the umbilical cord, which is also known as single umbilical artery (SUA). SUA is a condition where there is only one umbilical artery instead of two, which can reduce blood flow and oxygen delivery to the fetus. SUA can be associated with congenital anomalies or growth restriction in some cases.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
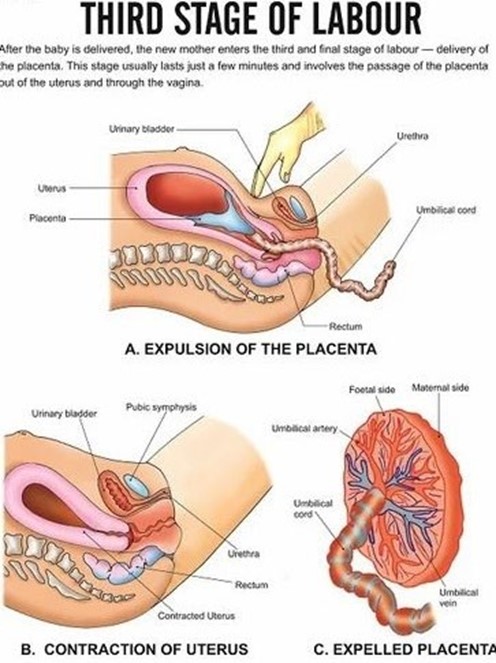
Choice A Reason: Assisting with the delivery of the placenta and ensuring that the fundus is contracted afterward. This is an appropriate action for the nurse to perform during the third stage of labor, as it helps complete the process of labor and prevent complications.
Choice B Reason: Palpating the woman's fundus for position and firmness. This is an action that is done after the delivery of the placenta, not during. It is important to monitor the fundal height, location, and consistency to assess uterine involution and bleeding.
Choice C Reason: Encouraging the woman to push with her contractions. This is an action that is done during the second stage of labor, not the third. The second stage of labor is the period from full cervical dilation to the birth of the baby. The nurse's role is to support and coach the woman to push effectively with her contractions.
Choice D Reason: Alleviating perineal discomfort with the application of ice packs. This is an action that is done after the delivery of the placenta, not during. It is a comfort measure that can reduce swelling, pain, and inflammation in the perineal area.
Correct Answer is D
Explanation
Choice A Reason: "My baby will always be smaller than other babies his age." This is an incorrect answer that indicates a misconception or pessimism about SGA newborns. SGA newborns may not always be smaller than other babies their age, as they may catch up in growth and development with appropriate nutrition and care. SGA newborns may have different growth paterns depending on the cause and timing of their growth restriction.
Choice B Reason: "My baby will be okay as long as he has frequent feedings." This is an incorrect answer that indicates an oversimplification or optimism about SGA newborns. SGA newborns may not be okay with just frequent feedings, as they may have other problems or complications that require medical atention and intervention. SGA newborns may have increased nutritional needs and feeding difficulties due to low birth weight, poor suck-swallow coordination, or oral aversion.
Choice C Reason: "My baby will need to stay in the hospital until he weighs 5 pounds." This is an incorrect answer that indicates a misunderstanding or confusion about SGA newborns. SGA newborns may not need to stay in the hospital until they weigh 5 pounds, as they may be discharged earlier or later depending on their condition and readiness for home care. SGA newborns may have different criteria for discharge based on their gestational age, weight gain, feeding tolerance, temperature stability, and absence of complications.
Choice D Reason: "My baby can get cold easily, may have low blood sugar, and may have trouble breathing." This is because this statement by the parents indicates that they understand some of the common problems and complications that SGA newborns may face. SGA newborns are those who weigh less than the 10th percentile for their gestational age, which can be due to intrauterine growth restriction (IUGR) or constitutional factors. SGA newborns may have difficulties with thermoregulation, glucose metabolism, and respiratory function due to inadequate fat stores, glycogen reserves, and surfactant production.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
