Why is it important for the nurse to assess the bladder regularly and encourage the laboring client to void every 2 hours?
Select one:
Frequent voiding encourages sphincter control.
A full bladder impedes oxygen flow to the fetus.
Frequent voiding prevents bruising of the bladder.
A full bladder can impede fetal descent.
The Correct Answer is D
Choice A Reason: Frequent voiding encourages sphincter control. This is an incorrect statement that has no relevance to labor and delivery. Sphincter control refers to the ability to contract and relax the muscles that control urination and defecation. It is not affected by frequent voiding.
Choice B Reason: A full bladder impedes oxygen flow to the fetus. This is an incorrect statement that confuses a full bladder with a prolapsed cord. A prolapsed cord is a condition where the umbilical cord slips through the cervix before the baby and becomes compressed by the fetal head, which can reduce oxygen flow to the fetus. A full bladder does not affect oxygen flow to the fetus.
Choice C Reason: Frequent voiding prevents bruising of the bladder. This is an incorrect statement that exaggerates the effect of a full bladder on the bladder wall. A full bladder may cause some pressure or discomfort on the bladder, but it does not cause bruising or damage.
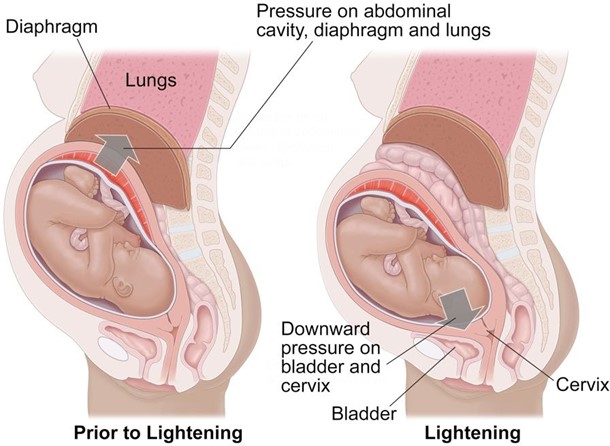
Choice D Reason: A full bladder can impede fetal descent. This is a correct statement that explains why it is important for the nurse to assess the bladder regularly and encourage the laboring client to void every 2 hours.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: Preterm infant. This is an incorrect answer that confuses TTN with another respiratory condition called respiratory distress syndrome (RDS). RDS is a serious condition where the newborn's lungs are immature and lack sufficient surfactant, which is a substance that reduces surface tension and prevents alveolar collapse. RDS can cause respiratory distress, hypoxia, acidosis, and organ failure. It is more common in preterm infants, especially those born before 37 weeks' gestation.
Choice B Reason: Female infant. This is an incorrect answer that has no evidence or rationale to support it. TTN does not have a gender preference or difference in incidence or severity.
Choice C Reason: GBS status of mother. This is an incorrect answer that relates to another respiratory complication called early-onset neonatal sepsis (EONS). EONS is a bacterial infection that occurs within 72 hours after birth, which can affect multiple organs and systems in the newborn. EONS can be caused by group B streptococcus (GBS), which is a common bacterium that colonizes in some women's vagina or rectum. GBS can be transmited to the newborn during delivery and cause pneumonia, meningitis, or septic shock.
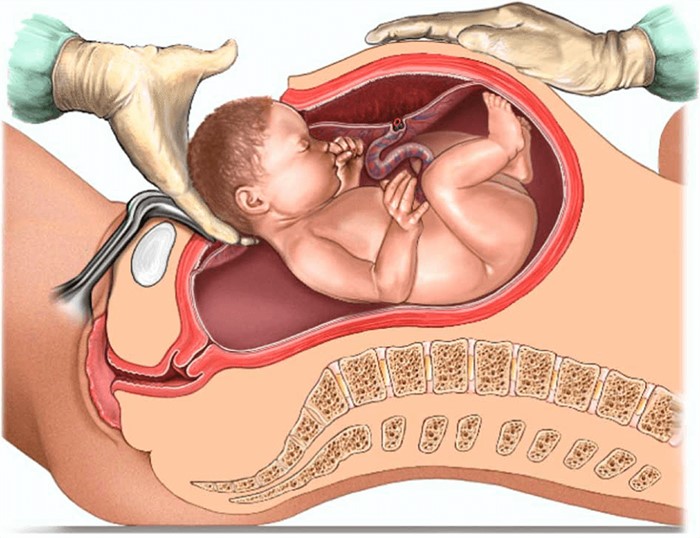
Choice D Reason: Cesarean section. This is because cesarean section is a risk factor for TTN, which is a mild respiratory problem that results from delayed clearance of fetal lung fluid after birth. TTN causes rapid breathing, nasal flaring, grunting, and mild cyanosis. It usually resolves within 24 to 48 hours after birth. Cesarean section can increase the risk of TTN because it bypasses the normal process of labor, which helps squeeze out some of the fluid from the fetal lungs.
Correct Answer is D
Explanation
Choice A Reason: About 1 of every 5 women will experience abuse in her lifetime is a statistic that shows the prevalence of domestic violence, but it does not address the question of what the nurse should emphasize to the group of women.
Choice B Reason: When women go back to the situation after the abuser has calmed down, things will be beter is a false statement that reflects the cycle of abuse, where the abuser may apologize and promise to change after a violent episode, but then repeat the same behavior later. This does not help the women understand their situation or seek help.
Choice C Reason: The victimized woman can easily leave the situation is a false statement that ignores the many barriers and challenges that women face when trying to escape from domestic violence, such as fear, isolation, financial dependence, lack of support, legal issues, and threats from the abuser. This does not empower the women or provide them with realistic options.
Choice D Reason: The violence will not stop or decrease if the woman becomes pregnant is a true statement that highlights the danger of staying in an abusive relationship during pregnancy. Domestic violence can increase the risk of miscarriage, preterm birth, low birth weight, placental abruption, fetal injury, and maternal death. This may motivate the women to seek safety and protection for themselves and their unborn children.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
