A woman is at 32 weeks' gestation. Her fundal height measurement at this clinic appointment is 26 centimeters. After reviewing her ultrasound results, the health care provider asks the nurse to schedule the client for a series of ultrasounds to be done every 2 weeks. The nurse should ensure that the client understands that the main purpose for this is to:
Select one:
Rule out a suspected hydatidiform mole.
Assess for congenital anomalies.
Determine fetal presentation.
Monitor fetal growth.
The Correct Answer is D
Choice A Reason: Rule out a suspected hydatidiform mole. This is an incorrect answer that describes an unlikely condition for this client. A hydatidiform mole is a type of gestational trophoblastic disease where abnormal placental tissue develops instead of a normal fetus. A hydatidiform mole can cause vaginal bleeding, hyperemesis gravidarum (severe nausea and vomiting), preeclampsia, and hyperthyroidism. A hydatidiform mole usually causes a fundal height measurement that is larger than expected for gestational age, not smaller.
Choice B Reason: Assess for congenital anomalies. This is an incorrect answer that implies that the client has not had a previous ultrasound to screen for fetal anomalies. Congenital anomalies are structural or functional defects that are present at birth, such as cleft lip, spina bifida, or Down syndrome. Ultrasound can detect some congenital anomalies by visualizing the fetal anatomy and morphology. However, ultrasound screening for fetal anomalies is usually done between 18 and 22 weeks of gestation, not at 32 weeks.
Choice C Reason: Determine fetal presentation. This is an incorrect answer that suggests that the client has an uncertain fetal presentation. Fetal presentation is the part of the fetus that is closest to the cervix, such as vertex (head), breech (butocks or feet), or transverse (shoulder). Fetal presentation can affect the mode and outcome of delivery. Ultrasound can determine fetal presentation by locating the fetal head and spine. However, fetal presentation can also be assessed by abdominal palpation or vaginal examination, which are simpler and less invasive methods.
Choice D Reason: Monitor fetal growth. This is because fundal height measurement is a method of estimating fetal size and gestational age by measuring the distance from the pubic symphysis to the top of the uterus (fundus) in centimeters. A fundal height measurement that is significantly smaller or larger than expected for gestational age may indicate intrauterine growth restriction (IUGR) or macrosomia, respectively. IUGR means that the fetal growth is slower than expected for gestational age, which can increase the risk of fetal distress, hypoxia, acidosis, and stillbirth. Macrosomia means that the fetal weight is higher than expected for gestational age, which can increase the risk of birth injuries, shoulder dystocia, cesarean delivery, and hypoglycemia. Ultrasound is a more accurate way of assessing fetal size and growth by measuring various parameters such as biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), and femur length (FL). Ultrasound can also detect other factors that may affect fetal growth such as placental function, amniotic fluid volume, umbilical cord blood flow, and fetal anomalies.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason: Pulmonary edema is a condition where fluid accumulates in the lungs, causing shortness of breath and difficulty breathing. It can occur in preeclampsia due to increased blood pressure and fluid retention, but it is not a definitive sign of eclampsia.
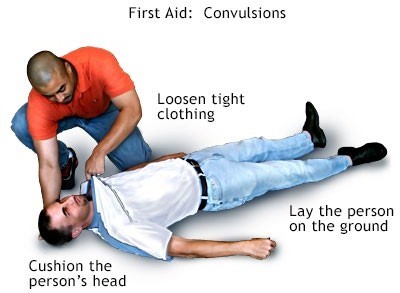
Choice B Reason: Convulsion (seizure) is a sudden, involuntary contraction of muscles that can cause loss of consciousness, shaking, and twitching. It is the main symptom of eclampsia and distinguishes it from preeclampsia.
Choice C Reason: Renal failure is a condition where the kidneys fail to filter waste products from the blood, resulting in high levels of creatinine and urea. It can occur in preeclampsia due to reduced blood flow to the kidneys, but it is not a specific indicator of eclampsia.
Choice D Reason: Retinal edema is a condition where fluid leaks into the retina, causing blurred vision and flashes of light. It can occur in preeclampsia due to increased blood pressure and damage to the blood vessels in the eye, but it is not a characteristic feature of eclampsia.
Correct Answer is C
Explanation
Choice A Reason: Obtain a bilirubin level. This is an incorrect answer that indicates an irrelevant and unnecessary nursing action for a newborn with tremors or jiteriness. Obtaining a bilirubin level is a nursing action that is indicated for a newborn with jaundice (yellowish discoloration of the skin and mucous membranes), which can occur due to increased bilirubin production or decreased bilirubin excretion. Jaundice does not cause tremors or jiteriness in newborns.
Choice B Reason: Place a pulse oximeter on the newborn. This is an incorrect answer that suggests an inappropriate and insufficient nursing action for a newborn with tremors or jiteriness. Placing a pulse oximeter on the newborn is a nursing action that measures oxygen saturation and heart rate, which can indicate hypoxia (low oxygen level) or distress in newborns. Hypoxia can cause tremors or jiteriness in newborns, but it is not the only or most likely cause. Placing a pulse oximeter on the newborn does not provide enough information to diagnose or treat hypoglycemia.
Choice C Reason: Obtain a blood glucose level. This is because tremors or jiteriness are common signs of hypoglycemia (low blood glucose) in newborns, which can occur due to various factors such as prematurity, maternal diabetes, infection, or cold stress. Hypoglycemia can cause neurological damage or death if not treated promptly and effectively. Obtaining a blood glucose level is a nursing action that has the highest priority for a newborn with tremors or jiteriness, as it can confirm the diagnosis and guide the treatment.
Choice D Reason: Take the newborn's vital signs. This is an incorrect answer that implies an inadequate and delayed nursing action for a newborn with tremors or jiteriness. Taking the newborn's vital signs is a nursing action that monitors temperature, pulse, respiration, and blood pressure, which can indicate general health status and stability in newborns. Taking the newborn's vital signs may reveal signs of hypoglycemia, such as hypothermia, tachycardia, tachypnea, or hypotension, but it is not a specific or definitive test for hypoglycemia. Taking the newborn's vital signs may also waste valuable time that could be used to obtain a blood glucose level and initiate treatment.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
