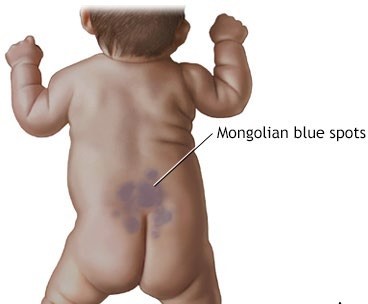
During a physical assessment of a newborn, the nurse observes bluish markings across the newborn's lower back. The nurse interprets this finding as:
Select one:
Milia.
Dermal melanosis.
Stork bites.
Birth trauma.
The Correct Answer is B
Choice A Reason: Milia. This is an incorrect answer that describes a different skin condition. Milia are tiny white or yellow cysts that appear on the nose, chin, or cheeks of newborns. They are caused by the retention of keratin in the sebaceous glands or hair follicles. They usually disappear within a few weeks without treatment.
Choice B Reason: Dermal melanosis. This is a correct answer that explains the finding of bluish markings across the newborn's lower back. Dermal melanosis. This is because dermal melanosis, also known as Mongolian spots, is a common benign skin condition that affects newborns of Asian, African, or Hispanic descent. It is characterized by bluish-gray or brown patches of pigmentation on the lower back, butocks, or extremities. It is caused by the migration of melanocytes from the neural crest to the dermis during embryonic development. It usually fades by 2 to 4 years of age.
Choice C Reason: Stork bites. This is an incorrect answer that refers to another skin condition. Stork bites, also known as salmon patches or nevus simplex, are flat pink or red marks that appear on the forehead, eyelids, nose, upper lip, or nape of the neck of newborns. They are caused by dilated capillaries in the superficial dermis. They usually fade by 18 months of age.
Choice D Reason: Birth trauma. This is an incorrect answer that implies an injury or damage to the newborn's skin or tissues during labor and delivery. Birth trauma can cause bruises, abrasions, lacerations, fractures, or nerve injuries. It is not related to bluish markings on the lower back.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: Retained placental fragments. This is an incorrect answer that refers to a different cause of late postpartum hemorrhage, which is less common than uterine atony. Retained placental fragments are pieces of placenta that remain atached to the uterine wall after delivery, which prevent uterine contraction and involution, and provide a source of bleeding and infection. Retained placental fragments can be caused by abnormal placentation (such as placenta accreta), manual removal of placenta, or incomplete separation of placenta.
Choice B Reason: Cervical or vaginal lacerations. This is an incorrect answer that refers to a different cause of late postpartum hemorrhage, which is more likely to cause early postpartum hemorrhage than late postpartum hemorrhage. Cervical or vaginal lacerations are tears or cuts in the cervix or vagina that occur during delivery, which can cause bleeding from the damaged blood vessels. Cervical or vaginal lacerations can be caused by rapid or instrumental delivery, large or malpositioned fetus, or episiotomy.
Choice C Reason: Uterine inversion. This is an incorrect answer that refers to a different cause of late postpartum hemorrhage, which is rare and life-threatening. Uterine inversion is a condition where the uterus turns inside out and protrudes through the cervix and vagina after delivery, which can cause massive bleeding and shock. Uterine inversion can be caused by excessive traction on the umbilical cord, fundal pressure, or uterine relaxation.
Choice D Reason: Uterine atony. This is because uterine atony is a condition where the uterus fails to contract and retract after delivery, which leads to bleeding from the placental site. Uterine atony is the most common cause of late postpartum hemorrhage, accounting for about 75% of cases. Late postpartum hemorrhage is excessive bleeding from the uterus or genital tract that occurs more than 24 hours but less than 12 weeks after delivery. Late postpartum hemorrhage can be caused by retained placental fragments, subinvolution of the uterus, infection, or coagulation disorders.
Correct Answer is D
Explanation
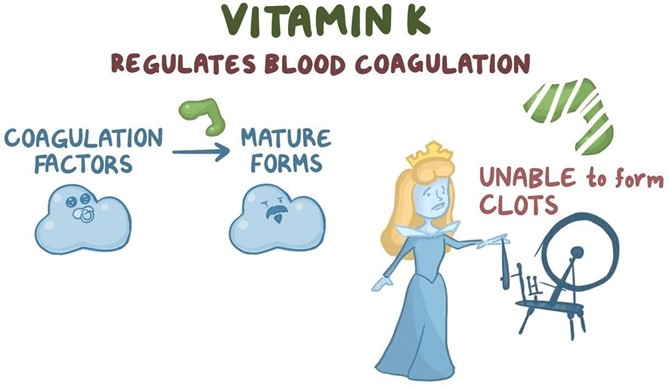
Choice A Reason: Vitamin K will increase erythropoiesis. This is an incorrect statement that confuses vitamin K with erythropoietin. Erythropoietin is a hormone that stimulates red blood cell production in the bone marrow. Vitamin K does not affect erythropoiesis.
Choice B Reason: Vitamin K will enhance bilirubin breakdown. This is an incorrect statement that confuses vitamin K with phototherapy. Phototherapy is a treatment that exposes the newborn's skin to light, which converts bilirubin into water-soluble forms that can be excreted by the liver and kidneys. Bilirubin is a yellow pigment that results from the breakdown of red blood cells. High levels of bilirubin can cause jaundice and brain damage in newborns. Vitamin K does not affect bilirubin metabolism.
Choice C Reason: Vitamin K will stop Rh sensitization. This is an incorrect statement that confuses vitamin K with Rh immune globulin. Rh immune globulin is an injection given to Rh-negative mothers who deliver Rh-positive babies, to prevent them from developing antibodies against Rh-positive blood cells in future pregnancies. Rh sensitization is a condition where the mother's immune system atacks the baby's blood cells, causing hemolytic disease of the newborn. Vitamin K does not affect Rh sensitization.
Choice D Reason: Vitamin K will promote blood clotting ability. This is a correct statement that explains the rationale for administering vitamin K as prophylaxis to newborns. Vitamin K is essential for the synthesis of clotting factors in the liver. Newborns have low levels of vitamin K at birth due to poor placental transfer and lack of intestinal bacteria that produce vitamin K. Therefore, they are at risk of bleeding disorders such as hemorrhagic disease of the newborn.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
