Narcotic analgesia is administered to a laboring client at 10:00 a.m. The infant is delivered at 10:35 A.M. The nurse would anticipate that the narcotic analgesia could:
Select one:
Enhance uterine contractions.
Be used in place of preoperative sedation.
Result in neonatal respiratory depression.
Prevent the need for anesthesia with an episiotomy.
The Correct Answer is C
Choice A Reason: Enhance uterine contractions. This is an incorrect answer that contradicts the effect of narcotic analgesia on uterine activity. Narcotic analgesia can reduce uterine contractions by decreasing maternal catecholamine levels, which can prolong labor or increase bleeding.
Choice B Reason: Be used in place of preoperative sedation. This is an irrelevant answer that does not apply to this scenario. Preoperative sedation is a medication given before surgery to reduce anxiety, pain, or nausea. Narcotic analgesia can be used as a preoperative sedative, but it is not related to labor or delivery.
Choice C Reason: Result in neonatal respiratory depression. This is because narcotic analgesia can cross the placenta and affect the fetal central nervous system, which can cause decreased respiratory drive, apnea, bradycardia, or hypotonia in the newborn. The risk of neonatal respiratory depression is higher when narcotic analgesia is administered close to delivery, as there is less time for placental clearance or maternal metabolism.
Choice D Reason: Prevent the need for anesthesia with an episiotomy. This is an inaccurate answer that overestimates the effect of narcotic analgesia on perineal pain. Narcotic analgesia can provide some relief of labor pain, but it does not block pain sensation completely or locally. An episiotomy is a surgical incision made in the perineum to enlarge the vaginal opening during delivery, which requires local anesthesia or regional anesthesia (such as epidural or spinal). Narcotic analgesia does not prevent or replace anesthesia with an episiotomy.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason: Daily weight. This is an incorrect answer that indicates a valid parameter to assess hydration status. Daily weight is a measure of the body mass that can reflect changes in fluid balance. Daily weight can help detect fluid loss or gain in premature infants, who are more prone to dehydration or overhydration due to immature renal function and high insensible water loss.
Choice B Reason: Consistency of stool. This is an incorrect answer that indicates a valid parameter to assess hydration status. Consistency of stool is a measure of the texture and form of feces that can reflect changes in fluid intake and absorption. Consistency of stool can help identify diarrhea or constipation in premature infants, who are more susceptible to gastrointestinal problems such as necrotizing enterocolitis or feeding intolerance.
Choice C Reason: Volume of urine output. This is an incorrect answer that indicates a valid parameter to assess hydration status. Volume of urine output is a measure of the amount of urine produced and excreted by the kidneys that can reflect changes in fluid balance and renal function. Volume of urine output can help monitor hydration status and kidney function in premature infants, who are more vulnerable to fluid overload or deficit and renal impairment.
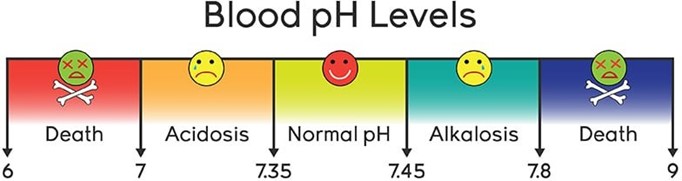
Choice D Reason: Blood pH. This is because blood pH is a measure of the acidity or alkalinity of the blood, which reflects the balance between carbon dioxide and bicarbonate in the body. Blood pH is not a direct indicator of hydration status, which refers to the amount of water and electrolytes in the body. Hydration status can affect blood pH, but blood pH can also be influenced by other factors such as respiratory or metabolic disorders.
Correct Answer is B
Explanation
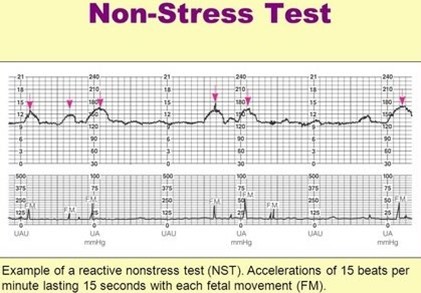
Choice A Reason: A fetal heart rate baseline of 140 with one acceleration to 155 for 15 seconds within 30 minutes. This is an incorrect answer that indicates a non-reactive NST, which is a test that does not meet the criteria for a reactive NST. A non-reactive NST may suggest fetal hypoxia, distress, or sleep, but it does not necessarily indicate a problem. A non-reactive NST may require further testing or stimulation to elicit a reactive result.
Choice B Reason A fetal heart rate baseline of 140 with two accelerations to 160 for 15 seconds within 20 minutes. This is because this strip meets the criteria for a reactive NST, which is a non-invasive test that evaluates fetal well- being and oxygenation by measuring the fetal heart rate response to fetal movements. A reactive NST is defined as having at least two accelerations of the fetal heart rate that are at least 15 beats per minute above the baseline and last for at least 15 seconds within a 20-minute period.
Choice C Reason: A fetal heart rate baseline of 130 with two accelerations to 135 for 15 seconds within 20 minutes. This is an incorrect answer that indicates a non-reactive NST, which is a test that does not meet the criteria for a reactive NST. The accelerations in this strip are not sufficient in amplitude, as they are only 5 beats per minute above the baseline, instead of at least 15 beats per minute.
Choice D Reason: A fetal heart rate baseline of 150 with two accelerations to 160 for 10 seconds within 20 minutes. This is an incorrect answer that indicates a non-reactive NST, which is a test that does not meet the criteria for a reactive NST. The accelerations in this strip are not sufficient in duration, as they last only for 10 seconds, instead of at least 15 seconds.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
