When the nurse is assessing a postpartum client approximately 6 hours after delivery, which finding would warrant further investigation?
Select one:
Moderate amounts of deep red lochia.
Sweating while afebrile.
Voiding 350 mL of blood-tinged urine.
Heart rate of 115 beats/minute.
The Correct Answer is D
Choice A Reason: Moderate amounts of deep red lochia. This is not a finding that would warrant further investigation, but rather a normal finding for the early postpartum period. Lochia is the vaginal discharge that occurs after delivery, which consists of blood, mucus, and tissue from the uterus. Lochia is usually deep red in color and moderate in amount for the first few days after delivery.
Choice B Reason: Sweating while afebrile. This is not a finding that would warrant further investigation, but rather a common occurrence in the postpartum period. Sweating is a mechanism of thermoregulation that helps the body eliminate excess fluid and electrolytes that were retained during pregnancy. Sweating does not necessarily indicate fever or infection.
Choice C Reason: Voiding 350 mL of blood-tinged urine. This is not a finding that would warrant further investigation, but rather an expected outcome for the postpartum period. Voiding large amounts of urine is normal in the postpartum period, as the body eliminates the excess fluid that was accumulated during pregnancy. Blood-tinged urine may be due to trauma or irritation of the urinary tract during labor or delivery, which usually resolves within a few days.
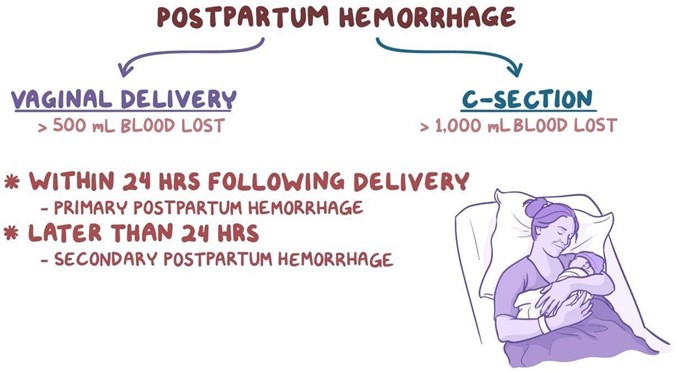
Choice D Reason: Heart rate of 115 beats/minute. This is because a heart rate of 115 beats/minute is higher than the normal range for an adult, which is 60 to 100 beats/minute. A high heart rate may indicate postpartum hemorrhage, infection, pain, anxiety, or dehydration. The nurse should further assess the client for other signs and symptoms of these conditions and notify the physician if necessary.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: Contact the physician, as it indicates early DIC. This is an incorrect answer that confuses a low pulse rate with a high pulse rate. DIC stands for disseminated intravascular coagulation, which is a life-threatening condition where abnormal clotting and bleeding occur simultaneously in the body. DIC can occur as a complication of postpartum hemorrhage, infection, or placental abruption. DIC can cause tachycardia (high pulse rate), not bradycardia (low pulse rate).
Choice B Reason: Contact the physician, as it is a first sign of postpartum eclampsia. This is an incorrect answer that misinterprets a low pulse rate as a sign of hypertension. Postpartum eclampsia is a condition where seizures occur in a woman who has preeclampsia or eclampsia after delivery. Preeclampsia and eclampsia are characterized by high blood pressure and proteinuria in pregnancy. Postpartum eclampsia can cause hypertension (high blood pressure), not hypotension (low blood pressure).
Choice C Reason: Document the finding as it is a normal finding at this time. This is because a pulse rate of 60 beats per minute is within the normal range for an adult and may reflect a physiological adaptation to the postpartum period. During pregnancy, the maternal blood volume and cardiac output increase, which can elevate the pulse rate. After delivery, these parameters gradually return to pre-pregnancy levels, which can lower the pulse rate.
Choice D Reason: Obtain an order for a CBC, as it suggests postpartum anemia. This is an incorrect answer that assumes that a low pulse rate is caused by anemia. Anemia is a condition where the red blood cell count or hemoglobin level is lower than normal, which can impair oxygen delivery to the tissues. Anemia can occur in the postpartum period due to blood loss during delivery or poor nutritional intake during pregnancy. Anemia can cause tachycardia (high pulse rate), not bradycardia (low pulse rate).

Correct Answer is A
Explanation
Choice A Reason: Two arteries, one vein. This is because two arteries and one vein are the normal components of the umbilical cord, which is a structure that connects the fetus to the placenta and provides blood circulation between them. The umbilical cord carries oxygenated blood from the placenta to the fetus through the umbilical vein, and deoxygenated blood from the fetus to the placenta through the umbilical arteries.
Choice B Reason: Two veins, one artery. This is an incorrect answer that indicates an abnormal anatomy of the umbilical cord, which is known as single umbilical artery (SUA). SUA is a condition where there is only one umbilical artery instead of two, which can reduce blood flow and oxygen delivery to the fetus. SUA can be associated with congenital anomalies or growth restriction in some cases.
Choice C Reason: Two veins, two arteries. This is an incorrect answer that indicates an abnormal anatomy of the umbilical cord, which is known as double umbilical vein (DUV). DUV is a condition where there are two umbilical veins instead of one, which can increase blood flow and oxygen delivery to the fetus. DUV can be associated with fetal overgrowth or polycythemia in some cases.
Choice D Reason: One artery, one vein. This is an incorrect answer that indicates an abnormal anatomy of the umbilical cord, which is also known as single umbilical artery (SUA). SUA is a condition where there is only one umbilical artery instead of two, which can reduce blood flow and oxygen delivery to the fetus. SUA can be associated with congenital anomalies or growth restriction in some cases.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
