The nurse assesses a 1-day-old newborn. Which finding indicates that the newborn's oxygenation needs are not being met?
Select one:
Grunting and nasal flaring.
Acrocyanosis.
Abdominal breathing.
Respiratory rate of 54 breaths/minute.
The Correct Answer is A
Choice A Reason: Grunting and nasal flaring. These are signs of respiratory distress in newborns, which indicate that their oxygenation needs are not being met. Grunting and nasal flaring. This is because grunting and nasal flaring are signs of respiratory distress in newborns, which indicate inadequate oxygenation and ventilation. Grunting is a noise made by the newborn when exhaling, which reflects an atempt to keep the alveoli open and increase lung volume.
Nasal flaring is a widening of the nostrils when inhaling, which reflects an effort to reduce airway resistance and increase airflow.
Choice B Reason: Acrocyanosis. This is not a sign of respiratory distress in newborns, but rather a common condition called acrocyanosis. Acrocyanosis means bluish discoloration of the hands and feet due to poor peripheral circulation in response to cold exposure or stress. It does not affect oxygenation or ventilation and usually disappears within 24 to 48 hours after birth.
Choice C Reason: Abdominal breathing. This is not a sign of respiratory distress in newborns, but rather a normal patern of breathing for them. Abdominal breathing means that the newborn's abdomen rises and falls with each breath, which reflects the use of the diaphragm as the primary respiratory muscle.
Choice D Reason: Respiratory rate of 54 breaths/minute. This is not a sign of respiratory distress in newborns, but rather a normal range of respiratory rate for them. A normal respiratory rate for a newborn ranges from 40 to 60 breaths per minute.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is B
Explanation
Choice A Reason: Shoulder dystocia. This is an incorrect answer that describes a different obstetric complication. Shoulder dystocia is a condition where the baby's shoulder gets stuck behind the mother's pubic bone during delivery, which can cause nerve injury, fracture, or asphyxia to the baby. Shoulder dystocia does not cause fetal bradycardia, abdominal pain, or vaginal bleeding.
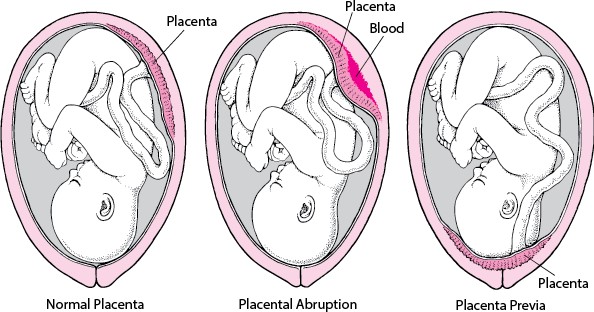
Choice B Reason: Placental abruption. This is a correct answer that explains the symptoms of fetal bradycardia, abdominal pain, and vaginal bleeding in a woman with a history of crack cocaine use. Placental abruption. This is because placental abruption is a condition where the placenta separates from the uterine wall before delivery, which can cause fetal distress, maternal hemorrhage, and shock. Placental abruption can be triggered by maternal hypertension, trauma, or substance abuse, such as crack cocaine.
Choice C Reason: Anaphylactoid syndrome of pregnancy. This is an incorrect answer that refers to a rare and fatal condition also known as amniotic fluid embolism. Anaphylactoid syndrome of pregnancy is a condition where amniotic fluid enters into the maternal bloodstream and causes an allergic reaction, which can lead to respiratory failure, cardiac arrest, coagulopathy, and coma. Anaphylactoid syndrome of pregnancy does not cause fetal bradycardia or vaginal bleeding.
Choice D Reason: Placenta previa. This is an incorrect answer that indicates another placental disorder. Placenta previa is a condition where the placenta covers or is near the cervix, which can cause painless bright red bleeding during pregnancy or labor. Placenta previa does not cause fetal bradycardia or abdominal pain.
Correct Answer is B
Explanation
Choice A Reason: Pulmonary edema is a condition where fluid accumulates in the lungs, causing shortness of breath and difficulty breathing. It can occur in preeclampsia due to increased blood pressure and fluid retention, but it is not a definitive sign of eclampsia.
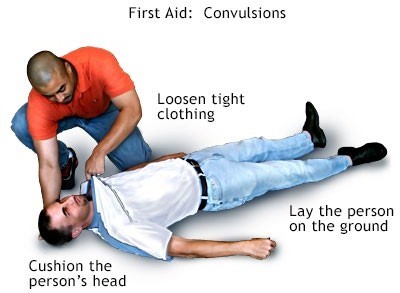
Choice B Reason: Convulsion (seizure) is a sudden, involuntary contraction of muscles that can cause loss of consciousness, shaking, and twitching. It is the main symptom of eclampsia and distinguishes it from preeclampsia.
Choice C Reason: Renal failure is a condition where the kidneys fail to filter waste products from the blood, resulting in high levels of creatinine and urea. It can occur in preeclampsia due to reduced blood flow to the kidneys, but it is not a specific indicator of eclampsia.
Choice D Reason: Retinal edema is a condition where fluid leaks into the retina, causing blurred vision and flashes of light. It can occur in preeclampsia due to increased blood pressure and damage to the blood vessels in the eye, but it is not a characteristic feature of eclampsia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
