The parents of a newborn who is being treated for bacterial septicemia ask the nurse why their baby didn't seem very ill. The best response of the nurse is:
Select one:
"You would have seen more symptoms if you had been looking more closely at your baby."
"A newborn's immune system isn't mature, so symptoms are subtle and can be hard to recognize."
"A high fever will always be present in sick newborns, including your baby."
"A mother's immunity usually protects the infant from illness, but not in this case."
The Correct Answer is B
Choice A Reason: "You would have seen more symptoms if you had been looking more closely at your baby." This is an inappropriate response that blames the parents for missing the signs of sepsis and does not explain the Reason for the subtle symptoms.
Choice B Reason: "A newborn's immune system isn't mature, so symptoms are subtle and can be hard to recognize." This is an appropriate response that educates the parents about the immunological basis of sepsis in newborns and reassures them that they are not at fault for not noticing the symptoms.
Choice C Reason: "A high fever will always be present in sick newborns, including your baby." This is an incorrect response that contradicts the fact that newborns may not develop fever in response to infection due to their immature immune systems.
Choice D Reason: "A mother's immunity usually protects the infant from illness, but not in this case." This is an inaccurate response that implies that the mother failed to provide adequate immunity to her baby and does not address the question of why the baby did not seem very ill.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
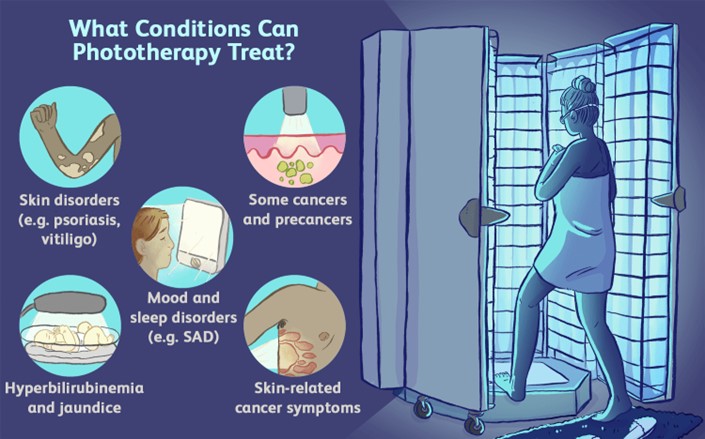
Choice A Reason: Applying Vaseline or lotion to newborn to maximize light absorption. This is an incorrect answer that indicates a contraindicated and harmful intervention that can interfere with phototherapy. Applying Vaseline or lotion to newborn can create a barrier or a reflective surface that can reduce the exposure and penetration of light to the skin, which can decrease the efficacy of phototherapy. Applying Vaseline or lotion to newborn can also cause skin irritation, infection, or burns, as it can trap heat and moisture under the light source.
Choice B Reason: Reducing the amount of fluid intake to 8 ounces daily. This is an incorrect answer that suggests a detrimental and dangerous intervention that can impair phototherapy. Reducing the amount of fluid intake to 8 ounces daily can cause dehydration, hypoglycemia, or electrolyte imbalance in newborns, which can worsen jaundice and increase the risk of complications such as kernicterus (brain damage due to high bilirubin levels). Reducing the amount of fluid intake to 8 ounces daily can also decrease the excretion of bilirubin through urine or stool, which can counteract the effect of phototherapy.
Choice C Reason: Keeping the newborn in the supine position. This is an incorrect answer that implies an incomplete and inadequate intervention that can limit phototherapy. Keeping the newborn in the supine position is a nursing action that involves placing the newborn on their back, which can expose their anterior body surface to light.
However, keeping the newborn in the supine position alone is not sufficient for phototherapy, as it does not expose their posterior body surface to light. The nurse should also reposition the newborn frequently to expose different body parts to light, such as their sides or abdomen.
Choice D Reason: Feeding every 3 hours to maximize intake of fluids and output. This is because feeding every 3 hours is a nursing intervention that can enhance the effectiveness and safety of phototherapy, which is a treatment that uses blue or white light to reduce the level of bilirubin in the blood. Bilirubin is a yellow pigment that is produced when red blood cells are broken down, which can cause jaundice (yellowish discoloration of the skin and mucous membranes) if it accumulates in excess. Phototherapy works by converting bilirubin into a water-soluble form that can be excreted through urine or stool. Feeding every 3 hours can increase the intake of fluids and calories, which can promote hydration, nutrition, and elimination of bilirubin.
Correct Answer is A
Explanation
Choice A Reason: Fetal movements are an indicator of fetal well-being. You should count twice a day, and you should feel ten fetal movements in 2 hours. This is because this response provides accurate and clear instructions on how to perform kick counts, which are a simple and non-invasive method of monitoring fetal activity and health. Kick counts can help detect changes in fetal movement paterns that may indicate fetal distress or hypoxia.
Choice B Reason: Here is a computer printed information packet on how to do kick counts. This is an insufficient answer that does not address the patient's question or demonstrate effective communication skills. Providing writen information alone may not ensure the patient's understanding or compliance with kick counts.
Choice C Reason: Fetal kick counts are not a reliable indicator of fetal well-being in the third trimester. This is an incorrect answer that contradicts the evidence and guidelines on kick counts. Kick counts are recommended for all pregnant women, especially in the third trimester, when fetal movements are more noticeable and consistent.
Choice D Reason: It is not important to do kick counts because you have a low-risk pregnancy. This is an incorrect answer that discourages the patient from performing kick counts and may give her a false sense of security. Kick counts are important for all pregnant women, regardless of their risk status, as they can help identify potential problems that may require further evaluation or intervention.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
