A woman who is 12 hours postpartum had a pulse rate around 80 beats per minute during pregnancy. Now, the nurse finds a pulse of 60 beats per minute. Which of these actions should the nurse take?
Select one:
Contact the physician, as it indicates early DIC.
Contact the physician, as it is a first sign of postpartum eclampsia.
Document the finding as it is a normal finding at this time.
Obtain an order for a CBC, as it suggests postpartum anemia.
The Correct Answer is C
Choice A Reason: Contact the physician, as it indicates early DIC. This is an incorrect answer that confuses a low pulse rate with a high pulse rate. DIC stands for disseminated intravascular coagulation, which is a life-threatening condition where abnormal clotting and bleeding occur simultaneously in the body. DIC can occur as a complication of postpartum hemorrhage, infection, or placental abruption. DIC can cause tachycardia (high pulse rate), not bradycardia (low pulse rate).
Choice B Reason: Contact the physician, as it is a first sign of postpartum eclampsia. This is an incorrect answer that misinterprets a low pulse rate as a sign of hypertension. Postpartum eclampsia is a condition where seizures occur in a woman who has preeclampsia or eclampsia after delivery. Preeclampsia and eclampsia are characterized by high blood pressure and proteinuria in pregnancy. Postpartum eclampsia can cause hypertension (high blood pressure), not hypotension (low blood pressure).
Choice C Reason: Document the finding as it is a normal finding at this time. This is because a pulse rate of 60 beats per minute is within the normal range for an adult and may reflect a physiological adaptation to the postpartum period. During pregnancy, the maternal blood volume and cardiac output increase, which can elevate the pulse rate. After delivery, these parameters gradually return to pre-pregnancy levels, which can lower the pulse rate.
Choice D Reason: Obtain an order for a CBC, as it suggests postpartum anemia. This is an incorrect answer that assumes that a low pulse rate is caused by anemia. Anemia is a condition where the red blood cell count or hemoglobin level is lower than normal, which can impair oxygen delivery to the tissues. Anemia can occur in the postpartum period due to blood loss during delivery or poor nutritional intake during pregnancy. Anemia can cause tachycardia (high pulse rate), not bradycardia (low pulse rate).

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
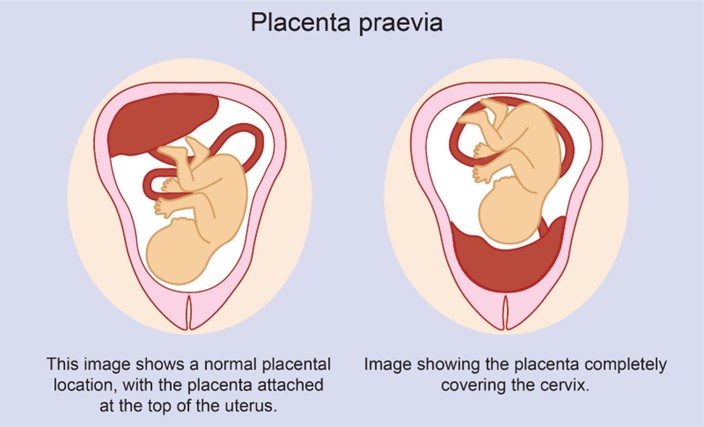
Choice A Reason: Partial placenta previa is a condition where the placenta partially covers the cervix. It usually does not resolve and may cause bleeding and complications during labor and delivery.
Choice B Reason: Complete placenta previa is a condition where the placenta completely covers the cervix. It is a serious condition that requires cesarean delivery and may cause life-threatening hemorrhage.
Choice C Reason: Marginal placenta previa is a condition where the edge of the placenta reaches the margin of the cervix. It may also cause bleeding and complications during labor and delivery.
Choice D Reason: Low-lying placenta previa is a condition where the placenta is near the cervix, but not covering it. It may resolve spontaneously as the uterus grows and the placenta moves upward.
Correct Answer is A
Explanation
Choice A Reason: "Our baby's newborn rash is from this syndrome." This is because this statement by a parent indicates that additional teaching is required, as it shows a misunderstanding or confusion about FAS and its manifestations. FAS is a condition that occurs when a woman consumes alcohol during pregnancy, which can affect the development and function of various organs and systems in the fetus and child. FAS can cause physical, behavioral, and cognitive problems such as facial abnormalities, growth retardation, learning difficulties, and atention deficits. FAS does not cause newborn rash, which is a common and benign condition that affects many newborns regardless of maternal alcohol intake. Newborn rash is also known as erythema toxicum neonatorum or baby acne, which is characterized by small red bumps or pustules on the face, chest, or back that usually disappear within a few weeks.
Choice B Reason: "His face looks like it does due to this problem." This is a correct answer that indicates adequate understanding of FAS and its features. Facial abnormalities are one of the characteristic signs of FAS, which include small eye openings, thin upper lip, flat nasal bridge, and smooth philtrum (the groove between the nose and upper lip).
Choice C Reason: "He can show signs of withdrawal from alcohol exposure like jiteriness, sweating, hyper reflexes, poor feeding and not sleeping well." This is a correct answer that indicates adequate understanding of FAS and its complications. Signs of withdrawal are possible effects of FAS, which occur when the fetus or newborn is exposed to alcohol in utero or through breast milk, which can cause neurotoxicity and dependency. Signs of withdrawal can include jiteriness, sweating, hyper reflexes, poor feeding, and not sleeping well, as well as irritability, seizures, or tremors.
Choice D Reason: "He is at risk of having intellectual disabilities, so we will need to get extra services to support him." This is a correct answer that indicates adequate understanding of FAS and its implications. Intellectual disabilities are potential outcomes of FAS, which affect the cognitive development and function of the child. Intellectual disabilities can cause problems with memory, Reasoning, language, and social skills. Extra services and support may be needed to help the child achieve their optimal potential and quality of life.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
