Following a normal spontaneous vaginal delivery (NSVD), a 28 year old G3 now P3 mother develops sudden onset shortness of breath, hypoxia and cyanosis. The delivery room nurse quickly recognizes these symptoms as possible:
Select one:
Manifestations of uteroplacental insufficiency.
Manifestations of prolapsed cord.
Manifestations of anaphylactoid syndrome of pregnancy.
Manifestations of an acute asthmatic episode.
The Correct Answer is C
Choice A Reason: Manifestations of uteroplacental insufficiency. This is an incorrect answer that describes a different condition that affects the fetus, not the mother. Uteroplacental insufficiency is a condition where the placenta fails to deliver adequate oxygen and nutrients to the fetus, which can result in fetal growth restriction, distress, or demise. Uteroplacental insufficiency does not cause shortness of breath, hypoxia, or cyanosis in the mother.
Choice B Reason: Manifestations of prolapsed cord. This is an incorrect answer that refers to another condition that affects the fetus, not the mother. Prolapsed cord is a condition where the umbilical cord slips through the cervix before the baby and becomes compressed by the fetal head, which can reduce oxygen flow to the fetus. Prolapsed cord does not cause shortness of breath, hypoxia, or cyanosis in the mother.
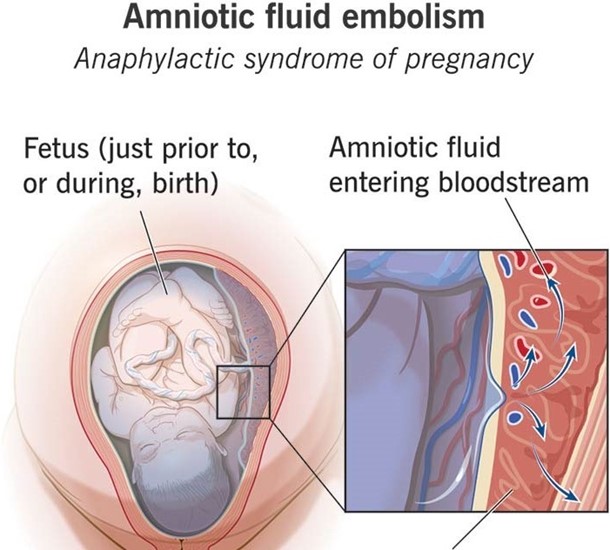
Choice C Reason: Manifestations of anaphylactoid syndrome of pregnancy. This is because anaphylactoid syndrome of pregnancy, also known as amniotic fluid embolism, is a rare and fatal condition where amniotic fluid enters into the maternal bloodstream and causes an allergic reaction, which can lead to respiratory failure, cardiac arrest, coagulopathy, and coma. Anaphylactoid syndrome of pregnancy can occur during or after labor and delivery, especially in cases of NSVD, multiparity, advanced maternal age, or placental abruption.
Choice D Reason: Manifestations of an acute asthmatic episode. This is an incorrect answer that assumes that the mother has a history of asthma or an allergic trigger. Asthma is a chronic inflammatory disorder of the airways that causes wheezing, coughing, chest tightness, and dyspnea. Asthma can be exacerbated by pregnancy or labor, but it is not a common cause of sudden onset respiratory distress in the postpartum period.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: IgG. This is an incorrect answer that refers to a different type of antibody that is not abundant in breast milk. IgG is a type of antibody that provides systemic immunity against various antigens. IgG is found in low concentrations in breast milk, as it does not cross the mammary epithelium easily. IgG can protect the infant from some infections, but it is mainly transferred from the mother to the fetus through the placenta during pregnancy.
Choice B Reason: IgE. This is an incorrect answer that refers to a different type of antibody that is not relevant to breast milk. IgE is a type of antibody that mediates allergic reactions and parasitic infections. IgE is found in very low concentrations in breast milk, as it does not have a significant role in mucosal immunity. IgE can trigger mast cells and basophils to release histamine and other inflammatory mediators, which can cause symptoms such as itching, swelling, or bronchoconstriction.
Choice C Reason: IgA. This is because IgA is a type of antibody that protects mucosal surfaces from pathogens and toxins. IgA is found in high concentrations in breast milk, especially in colostrum (the first milk produced after delivery). IgA can bind to bacteria and viruses in the infant's gastrointestinal tract and prevent them from ataching to the intestinal wall or crossing into the bloodstream. IgA can also enhance the infant's immune system by stimulating lymphoid tissue development and modulating inflammatory responses.
Choice D Reason: IgM. This is an incorrect answer that refers to a different type of antibody that is not abundant in breast milk. IgM is a type of antibody that activates complement system and agglutinates antigens. IgM is found in low concentrations in breast milk, as it does not cross the mammary epithelium easily due to its large size. IgM can protect the infant from some infections, but it is mainly produced by the infant's own immune system in response to exposure to antigens.
Correct Answer is D
Explanation
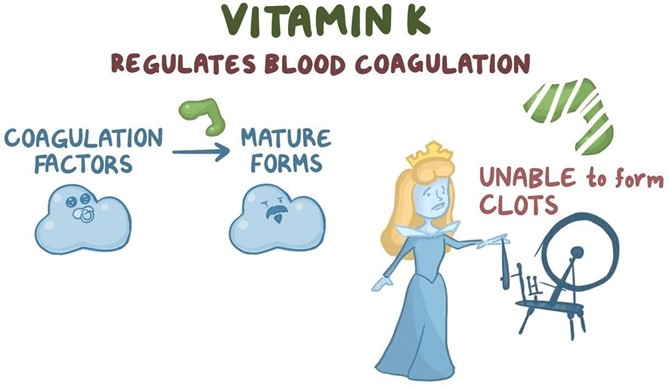
Choice A Reason: Vitamin K will increase erythropoiesis. This is an incorrect statement that confuses vitamin K with erythropoietin. Erythropoietin is a hormone that stimulates red blood cell production in the bone marrow. Vitamin K does not affect erythropoiesis.
Choice B Reason: Vitamin K will enhance bilirubin breakdown. This is an incorrect statement that confuses vitamin K with phototherapy. Phototherapy is a treatment that exposes the newborn's skin to light, which converts bilirubin into water-soluble forms that can be excreted by the liver and kidneys. Bilirubin is a yellow pigment that results from the breakdown of red blood cells. High levels of bilirubin can cause jaundice and brain damage in newborns. Vitamin K does not affect bilirubin metabolism.
Choice C Reason: Vitamin K will stop Rh sensitization. This is an incorrect statement that confuses vitamin K with Rh immune globulin. Rh immune globulin is an injection given to Rh-negative mothers who deliver Rh-positive babies, to prevent them from developing antibodies against Rh-positive blood cells in future pregnancies. Rh sensitization is a condition where the mother's immune system atacks the baby's blood cells, causing hemolytic disease of the newborn. Vitamin K does not affect Rh sensitization.
Choice D Reason: Vitamin K will promote blood clotting ability. This is a correct statement that explains the rationale for administering vitamin K as prophylaxis to newborns. Vitamin K is essential for the synthesis of clotting factors in the liver. Newborns have low levels of vitamin K at birth due to poor placental transfer and lack of intestinal bacteria that produce vitamin K. Therefore, they are at risk of bleeding disorders such as hemorrhagic disease of the newborn.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
