A postpartum client has a fourth-degree perineal laceration. The nurse would expect which of the following medications to be ordered?
Select one:
Docusate sodium (Colace).
Bromocriptine (Parlodel).
Ferrous sulfate (Feosol).
Methylergonovine (Methergine).
The Correct Answer is A
Choice A Reason: Docusate sodium (Colace). This is because docusate sodium is a stool softener that can prevent constipation and straining during defecation, which can aggravate or impair the healing of a perineal laceration. A fourth-degree perineal laceration is a severe tear that extends through the skin, muscles, perineal body, and anal sphincter into the rectal mucosa. It can occur during vaginal delivery due to factors such as fetal macrosomia, forceps use, or episiotomy.
Choice B Reason: Bromocriptine (Parlodel). This is an inappropriate medication for a postpartum client with a fourth- degree perineal laceration, as it has no effect on wound healing or pain relief. Bromocriptine is a dopamine agonist that can suppress lactation by inhibiting prolactin secretion. It is used for women who do not wish to breastfeed or who have medical contraindications to breastfeeding.
Choice C Reason: Ferrous sulfate (Feosol). This is an unnecessary medication for a postpartum client with a fourth- degree perineal laceration, unless she has iron deficiency anemia. Ferrous sulfate is an iron supplement that can treat or prevent anemia by increasing hemoglobin production and oxygen-carrying capacity. Anemia can occur in the postpartum period due to blood loss during delivery or poor nutritional intake during pregnancy.
Choice D Reason: Methylergonovine (Methergine). This is an irrelevant medication for a postpartum client with a fourth-degree perineal laceration, as it does not affect wound healing or pain relief. Methylergonovine is an ergot alkaloid that can stimulate uterine contractions and reduce postpartum bleeding. It is used for women who have uterine atony or hemorrhage.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A Reason: Contact the physician, as it indicates early DIC. This is an incorrect answer that confuses a low pulse rate with a high pulse rate. DIC stands for disseminated intravascular coagulation, which is a life-threatening condition where abnormal clotting and bleeding occur simultaneously in the body. DIC can occur as a complication of postpartum hemorrhage, infection, or placental abruption. DIC can cause tachycardia (high pulse rate), not bradycardia (low pulse rate).
Choice B Reason: Contact the physician, as it is a first sign of postpartum eclampsia. This is an incorrect answer that misinterprets a low pulse rate as a sign of hypertension. Postpartum eclampsia is a condition where seizures occur in a woman who has preeclampsia or eclampsia after delivery. Preeclampsia and eclampsia are characterized by high blood pressure and proteinuria in pregnancy. Postpartum eclampsia can cause hypertension (high blood pressure), not hypotension (low blood pressure).
Choice C Reason: Document the finding as it is a normal finding at this time. This is because a pulse rate of 60 beats per minute is within the normal range for an adult and may reflect a physiological adaptation to the postpartum period. During pregnancy, the maternal blood volume and cardiac output increase, which can elevate the pulse rate. After delivery, these parameters gradually return to pre-pregnancy levels, which can lower the pulse rate.
Choice D Reason: Obtain an order for a CBC, as it suggests postpartum anemia. This is an incorrect answer that assumes that a low pulse rate is caused by anemia. Anemia is a condition where the red blood cell count or hemoglobin level is lower than normal, which can impair oxygen delivery to the tissues. Anemia can occur in the postpartum period due to blood loss during delivery or poor nutritional intake during pregnancy. Anemia can cause tachycardia (high pulse rate), not bradycardia (low pulse rate).

Correct Answer is B
Explanation
Choice A Reason: Pulmonary edema is a condition where fluid accumulates in the lungs, causing shortness of breath and difficulty breathing. It can occur in preeclampsia due to increased blood pressure and fluid retention, but it is not a definitive sign of eclampsia.
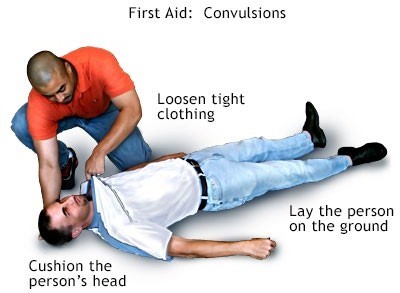
Choice B Reason: Convulsion (seizure) is a sudden, involuntary contraction of muscles that can cause loss of consciousness, shaking, and twitching. It is the main symptom of eclampsia and distinguishes it from preeclampsia.
Choice C Reason: Renal failure is a condition where the kidneys fail to filter waste products from the blood, resulting in high levels of creatinine and urea. It can occur in preeclampsia due to reduced blood flow to the kidneys, but it is not a specific indicator of eclampsia.
Choice D Reason: Retinal edema is a condition where fluid leaks into the retina, causing blurred vision and flashes of light. It can occur in preeclampsia due to increased blood pressure and damage to the blood vessels in the eye, but it is not a characteristic feature of eclampsia.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
