After the birth of a newborn, the nursing intervention that most effectively promotes parental atachment is: Select one:
Taking the newborn to the nursery for the initial assessment.
Allowing the mother a chance to rest without the baby immediately after delivery.
Placing the newborn under a radiant warmer to do the initial assessment.
Placing the newborn on the maternal abdomen and doing the initial assessment.
The Correct Answer is D
Choice A Reason: Taking the newborn to the nursery for the initial assessment. This is an ineffective intervention that disrupts parental atachment by separating the mother and the newborn. It also deprives the newborn of the benefits of skin to skin contact and breastfeeding.
Choice B Reason: Allowing the mother a chance to rest without the baby immediately after delivery. This is an unnecessary intervention that delays parental atachment by postponing the first contact between the mother and the newborn. It also ignores the mother's desire and readiness to hold and feed her baby.
Choice C Reason: Placing the newborn under a radiant warmer to do the initial assessment. This is an outdated intervention that hinders parental atachment by creating a physical barrier between the mother and the newborn. It also exposes the newborn to potential risks such as dehydration, hyperthermia, or eye damage.
Choice D Reason: Placing the newborn on the maternal abdomen and doing the initial assessment. This is because this intervention facilitates skin to skin contact, eye contact, and bonding between the mother and the newborn. It also enhances breastfeeding initiation, thermoregulation, and maternal-infant atachment.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
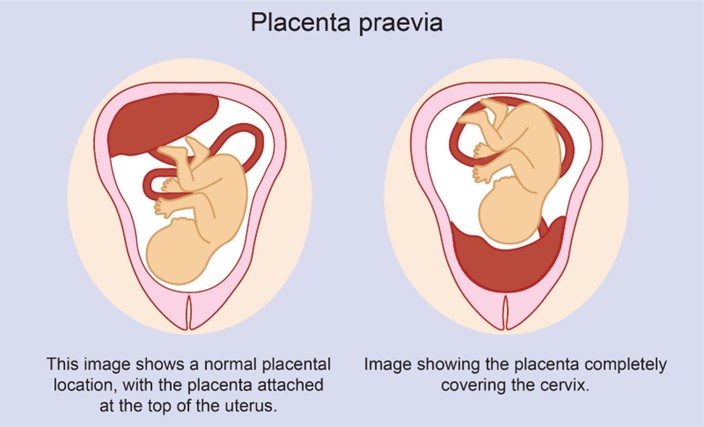
Choice A Reason: Partial placenta previa is a condition where the placenta partially covers the cervix. It usually does not resolve and may cause bleeding and complications during labor and delivery.
Choice B Reason: Complete placenta previa is a condition where the placenta completely covers the cervix. It is a serious condition that requires cesarean delivery and may cause life-threatening hemorrhage.
Choice C Reason: Marginal placenta previa is a condition where the edge of the placenta reaches the margin of the cervix. It may also cause bleeding and complications during labor and delivery.
Choice D Reason: Low-lying placenta previa is a condition where the placenta is near the cervix, but not covering it. It may resolve spontaneously as the uterus grows and the placenta moves upward.
Correct Answer is A
Explanation
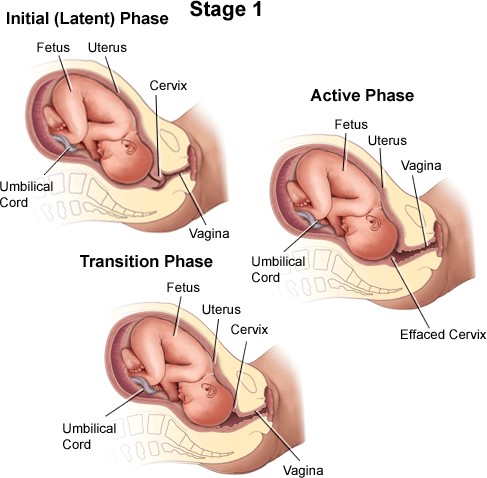
Choice A Reason: Latent phase of the first stage of labor. This is because this phase is characterized by mild and irregular contractions, slow cervical dilation (up to 4 cm), minimal cervical effacement (up to 40%), and minimal discomfort or pain. The latent phase is also known as the early phase or preparatory phase of labor.
Choice B Reason: Transition phase of the first stage of labor. This is an incorrect answer that describes a different phase with different characteristics. The transition phase is marked by strong and frequent contractions, rapid cervical dilation (from 8 to 10 cm), complete cervical effacement (100%), and intense discomfort or pain. The transition phase is also known as the terminal phase or acceleration phase of labor.
Choice C Reason: Perineal phase of the second stage of labor. This is an incorrect answer that refers to another stage and phase with different features. The second stage of labor begins with complete cervical dilation (10 cm) and ends with delivery of the baby. The perineal phase is the last part of the second stage, where the baby's head crowns and emerges through the vaginal opening.
Choice D Reason: Active phase of the first stage of labor. This is an incorrect answer that indicates another phase with different atributes. The active phase is characterized by moderate and regular contractions, progressive cervical dilation (from 4 to 8 cm), increased cervical effacement (from 40% to 80%), and increased discomfort or pain. The active phase is also known as the middle phase or dilatation phase of labor.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
