On arrival at the intensive care unit, a critically ill patient suffers respiratory arrest and is placed on mechanical ventilation. The physician orders pulse oximetry to monitor the patient’s arterial oxygen saturation (SaO₂) noninvasively. Which vital sign abnormality may alter pulse oximetry values?
Tachycardia
Hypotension
Tachypnea
Fever
The Correct Answer is B
Choice A: Tachycardia
Tachycardia, defined as a heart rate exceeding 100 beats per minute, can affect the accuracy of pulse oximetry readings. When the heart beats too quickly, it may not fill with enough blood between beats, leading to reduced perfusion and oxygen delivery to tissues. However, while tachycardia can influence the readings, it is not the most significant factor compared to hypotension.
Choice B: Hypotension
Hypotension, or low blood pressure, significantly impacts pulse oximetry accuracy. When blood pressure is low, there is reduced perfusion to peripheral tissues, including the extremities where pulse oximeters are typically placed. This reduced perfusion can lead to inaccurate readings, as the device may not detect sufficient blood flow to measure oxygen saturation accurately. Hypotension is a critical factor that can alter pulse oximetry values, making it the most relevant choice.
Choice C: Tachypnea
Tachypnea, or rapid breathing, can affect oxygen levels in the blood but does not directly interfere with the pulse oximeter’s ability to measure oxygen saturation. While it indicates respiratory distress and can lead to hypoxemia, the pulse oximeter can still provide accurate readings unless accompanied by other factors like low perfusion.
Choice D: Fever
Fever can cause peripheral vasodilation, which might theoretically affect pulse oximetry readings by altering blood flow to the extremities. However, this effect is generally minimal compared to the impact of hypotension. Fever alone is unlikely to cause significant inaccuracies in pulse oximetry measurements.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason:
Assessing the client’s gag reflex before giving any food or water is crucial after a bronchoscopy. The procedure involves the use of local anesthesia to numb the throat, which can impair the gag reflex and increase the risk of aspiration. Ensuring that the gag reflex has returned before allowing the client to eat or drink helps prevent choking and aspiration, which are serious complications.
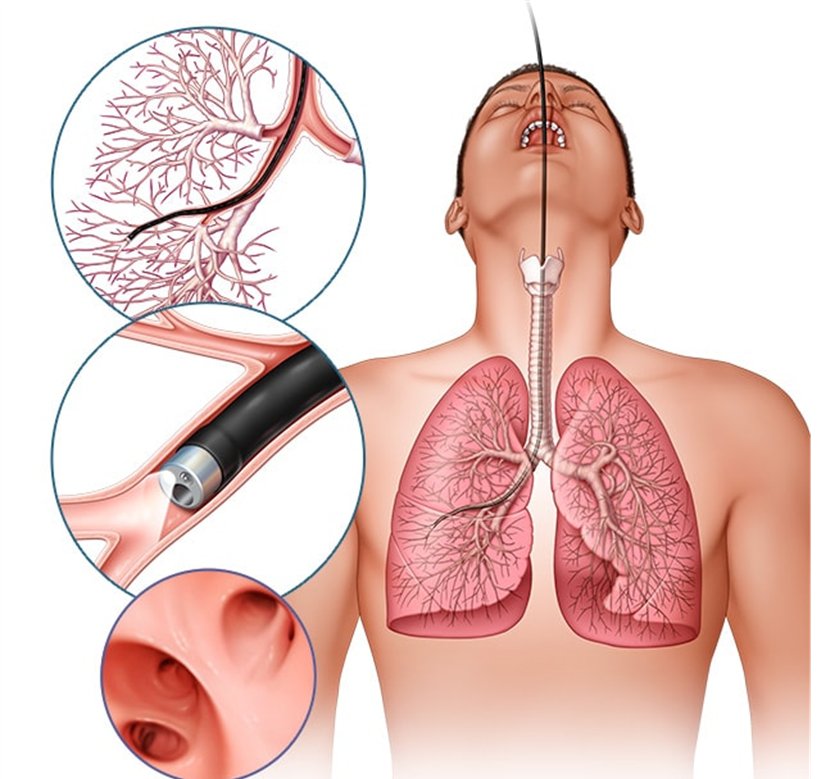
Choice B Reason:
Providing the client with ice chips instead of a drink of water is not the best initial action. While ice chips may seem like a safer option, they still pose a risk of aspiration if the gag reflex has not fully returned. The priority is to first assess the gag reflex to ensure the client can safely swallow.
Choice C Reason:
Contacting the primary healthcare provider and getting the appropriate orders is not necessary as the first action. The nurse can independently assess the gag reflex, which is a standard nursing practice after procedures involving throat anesthesia. If there are concerns after the assessment, then contacting the healthcare provider would be appropriate.
Choice D Reason:
Letting the client have a small sip to evaluate the ability to swallow is not safe without first assessing the gag reflex. This approach could lead to aspiration if the gag reflex has not returned. The initial step should always be to assess the gag reflex to ensure the client can safely swallow liquids.
Correct Answer is A
Explanation
Choice A: Metformin
Reason: Metformin is known to interact with contrast material, particularly iodinated contrast media, and can increase the risk of acute kidney injury (AKI). This interaction can lead to a condition known as contrast-induced nephropathy (CIN) or contrast-induced acute kidney injury (CI-AKI). Metformin is primarily excreted by the kidneys, and impaired renal function can lead to its accumulation, increasing the risk of lactic acidosis, a rare but serious complication. Therefore, it is generally recommended to withhold metformin before and after the administration of contrast media until renal function is confirmed to be normal.
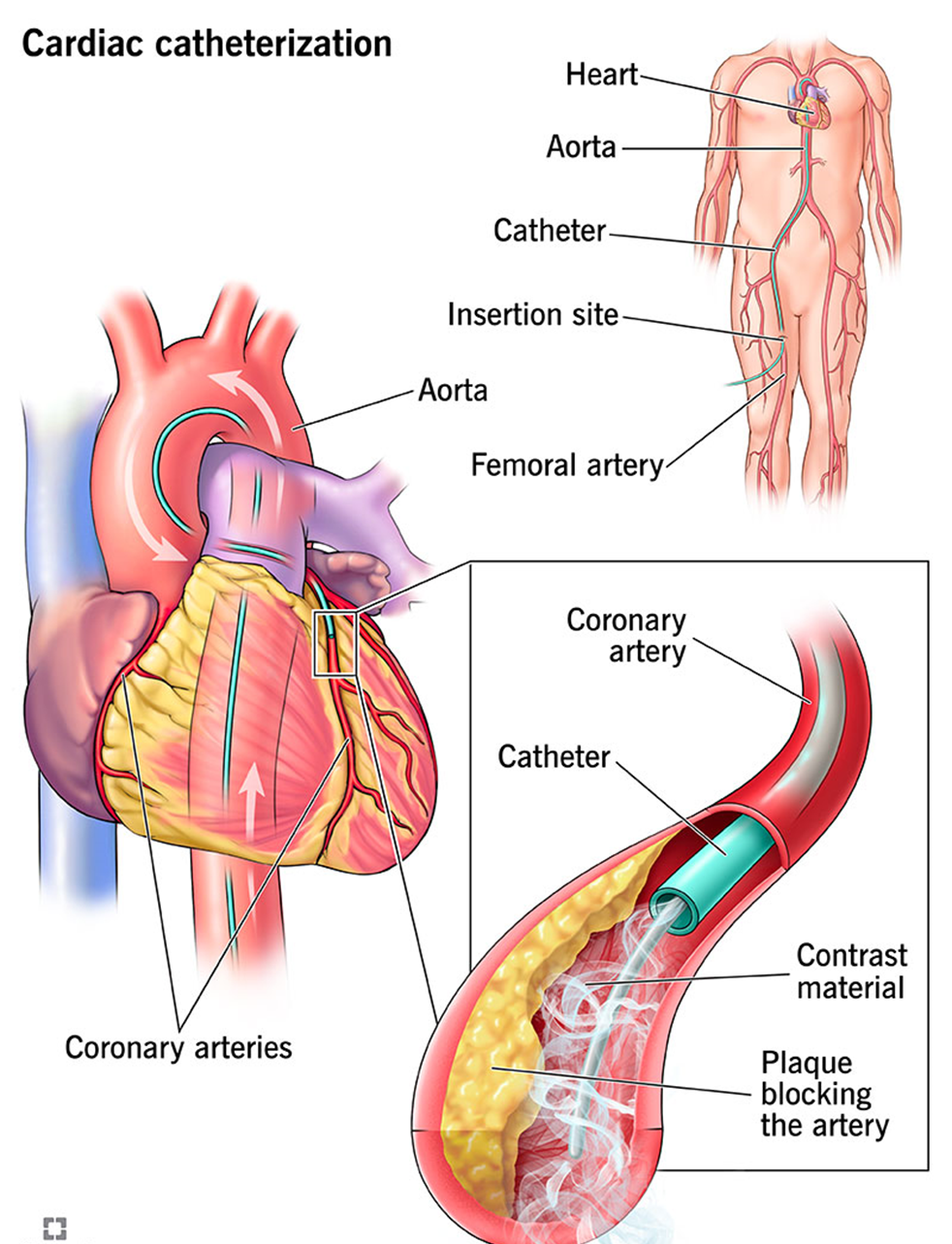
Choice B: Carvedilol
Reason: Carvedilol is a beta-blocker used to treat high blood pressure and heart failure. It does not have a known interaction with contrast media that would increase the risk of acute kidney injury. Carvedilol primarily affects the cardiovascular system and does not significantly impact renal function or interact with contrast agents.
Choice C: Nitroglycerin
Reason: Nitroglycerin is used to treat angina and other heart conditions by dilating blood vessels. It does not interact with contrast media in a way that would increase the risk of acute kidney injury. Nitroglycerin’s primary effects are on the cardiovascular system, and it does not have nephrotoxic properties.
Choice D: Atorvastatin
Reason: Atorvastatin is a statin used to lower cholesterol levels. While it can have effects on liver enzymes and muscle tissue, it does not interact with contrast media to increase the risk of acute kidney injury. Atorvastatin is metabolized by the liver and does not significantly impact renal function.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
