The nurse is caring for a client immediately following a cardioversion. What nursing actions are appropriate? (Select all that apply.)
Provide continued sedation.
Remove crash cart from the room.
Assess the chest for burns.
Ensure electrodes are in place for continued monitoring.
Document results of the procedure.
Correct Answer : C,D,E
Choice A Reason:
Provide continued sedation.
Providing continued sedation is not typically necessary after a cardioversion. The sedation used during the procedure is usually short-acting, and the client should begin to wake up shortly after the procedure is completed. Continuous sedation is not required unless there are specific medical reasons, which should be determined by the healthcare provider.
Choice B Reason:
Remove crash cart from the room.
The crash cart should remain in the room until the client is fully stable. Removing it immediately after the procedure is not advisable because the client may still be at risk for complications such as arrhythmias or other cardiac events. Keeping the crash cart nearby ensures that emergency equipment is readily available if needed.
Choice C Reason:
Assess the chest for burns.
Assessing the chest for burns is an important nursing action following a cardioversion. The electrical shock delivered during the procedure can cause burns on the skin where the electrodes were placed. It is essential to check for any signs of burns or skin irritation and provide appropriate care if needed.
Choice D Reason:
Ensure electrodes are in place for continued monitoring.
Ensuring that the electrodes are in place for continued monitoring is crucial. Continuous cardiac monitoring is necessary to observe the client’s heart rhythm and detect any potential complications or recurrence of arrhythmias. Proper placement and function of the electrodes are essential for accurate monitoring.
Choice E Reason:
Document results of the procedure.
Documenting the results of the procedure is a critical nursing action. Accurate documentation includes noting the client’s response to the cardioversion, any complications, and the current heart rhythm. This information is vital for ongoing care and communication with the healthcare team.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice A Reason:
Pronation of the hands.
Pronation of the hands is not typically associated with decorticate posturing. Decorticate posturing is characterized by the flexion of the arms and wrists, with the hands often clenched into fists. Pronation refers to the rotation of the hands so that the palms face downward, which is not a feature of decorticate posturing.
Choice B Reason:
Extension of the arms.
Extension of the arms is more characteristic of decerebrate posturing, not decorticate posturing. In decorticate posturing, the arms are flexed and held tightly to the chest, not extended. This flexion is due to damage to the cerebral hemispheres, which affects the corticospinal tract.
Choice C Reason:
External rotation of the lower extremities.
External rotation of the lower extremities is not a typical finding in decorticate posturing. In decorticate posturing, the legs are usually extended and rigid, with the toes pointed. External rotation would indicate a different type of posturing or neurological condition.
Choice D Reason:
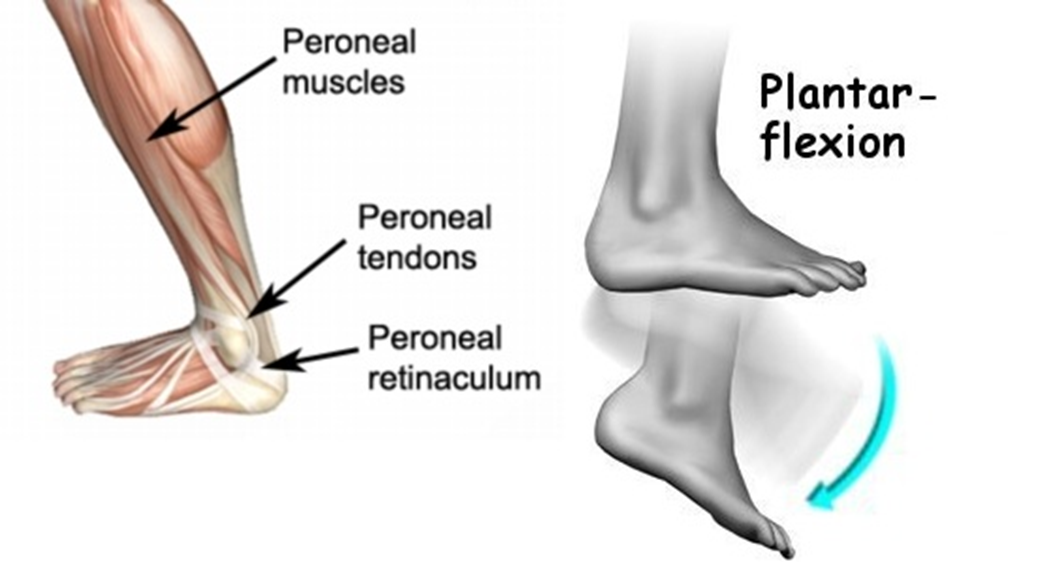
Plantar flexion of the legs.
Plantar flexion of the legs is a characteristic finding in decorticate posturing. This involves the toes pointing downward, which is a result of the increased muscle tone and reflexes due to the brain injury. This posture indicates severe damage to the brain, specifically the corticospinal tract.
Correct Answer is ["A","D","E"]
Explanation
Choice A Reason:
Cool, clammy skin is a common symptom in patients with atrial fibrillation, especially when the heart rate is very high. This symptom occurs due to decreased cardiac output, which leads to poor perfusion of the skin. When the heart is beating too fast, it doesn’t have enough time to fill properly, resulting in less blood being pumped out to the body. This can cause the skin to feel cool and clammy as the body tries to compensate for the reduced blood flow.
Choice B Reason:
Respiratory rate of 20 is within the normal range for adults, which is typically 12-20 breaths per minute. While it is important to monitor respiratory rate in patients with atrial fibrillation, a rate of 20 does not indicate any immediate distress or abnormality. Therefore, this choice is not particularly relevant to the assessment of a patient with a heart rate of 143 beats/min due to atrial fibrillation.
Choice C Reason:
Flushing of the skin is not a typical symptom associated with atrial fibrillation. Flushing can occur due to various reasons such as fever, anxiety, or certain medications, but it is not directly linked to the high heart rate or the irregular rhythm seen in atrial fibrillation. Therefore, this choice is not applicable in this context.
Choice D Reason:
Hypotension (low blood pressure) is a significant concern in patients with atrial fibrillation, especially when the heart rate is very high. The rapid heart rate can lead to decreased cardiac output, as the heart does not have enough time to fill properly between beats. This can result in lower blood pressure, which can cause symptoms such as dizziness, fainting, and fatigue. Monitoring blood pressure is crucial in managing patients with atrial fibrillation to prevent complications.
Choice E Reason:
Chest discomfort is a common symptom in patients with atrial fibrillation, particularly when the heart rate is very high. The irregular and rapid heart rate can cause the heart to work harder, leading to increased oxygen demand and potentially reduced oxygen supply to the heart muscle. This imbalance can result in chest pain or discomfort, which is a warning sign that the heart is under stress. It is important to assess and address chest discomfort promptly to prevent further cardiac complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
