What does the nurse recognize as clinical manifestations consistent with ascites? Select all that apply.
Stretch marks
Foul-smelling breath
Increased abdominal girth
Visible distended veins
Rapid weight gain
Correct Answer : C,D,E
Choice A reason: Stretch marks, also known as striae, are not specific to ascites. They can occur due to rapid weight gain or loss, pregnancy, or other conditions that cause the skin to stretch. While they may be present in individuals with ascites due to rapid abdominal expansion, they are not a primary clinical manifestation of ascites.
Choice B reason: Foul-smelling breath, or halitosis, is not a typical symptom of ascites. It can be associated with various conditions, including poor oral hygiene, gastrointestinal disorders, or liver disease, but it is not a direct indicator of ascites.
Choice C reason: Increased abdominal girth is a primary clinical manifestation of ascites. Ascites is characterized by the accumulation of fluid in the peritoneal cavity, leading to noticeable abdominal distension. This symptom is often accompanied by a feeling of fullness or bloating.
Choice D reason: Visible distended veins, particularly around the abdomen, can be a sign of ascites. This occurs due to increased pressure in the abdominal veins as a result of fluid accumulation. The veins become more prominent and visible under the skin.
Choice E reason: Rapid weight gain is another key indicator of ascites. The accumulation of fluid in the abdomen leads to a significant increase in body weight over a short period. This rapid weight gain is often one of the first signs that prompts further investigation for ascites.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A: He is NPO until the speech-language pathologist performs a swallowing evaluation.
When a client is admitted with a stroke, especially one affecting the left side, there is a significant risk of dysphagia, or difficulty swallowing. This can lead to choking and aspiration, which can cause pneumonia and other complications. Therefore, it is crucial to keep the client NPO (nothing by mouth) until a speech-language pathologist can perform a thorough swallowing evaluation. This ensures that the client can safely swallow without the risk of aspiration. The speech-language pathologist will assess the client’s ability to swallow different textures and consistencies of food and liquids and provide recommendations for safe feeding.

Choice B: Be sure to sit him up when you are feeding him to make him feel more natural.
While sitting the client up during feeding is a good practice to reduce the risk of aspiration, it is not sufficient on its own for a client who has just had a stroke. Without a proper swallowing evaluation, feeding the client could still pose a significant risk. Therefore, this choice is not the most appropriate response.
Choice C: You may give him a full-liquid diet, but please avoid solid foods until he gets stronger.
A full-liquid diet might seem like a safer option, but it still poses a risk of aspiration if the client has dysphagia. Without a swallowing evaluation, it is not safe to assume that the client can handle even a full-liquid diet. Therefore, this choice is not appropriate.
Choice D: Just be sure to add some thickener in his liquids to prevent choking and aspiration.
Adding thickener to liquids can help some clients with dysphagia, but it is not a one-size-fits-all solution. The appropriate consistency of liquids should be determined by a speech-language pathologist after a swallowing evaluation. Therefore, this choice is not appropriate without a prior assessment.
Correct Answer is C
Explanation
Choice A Reason:
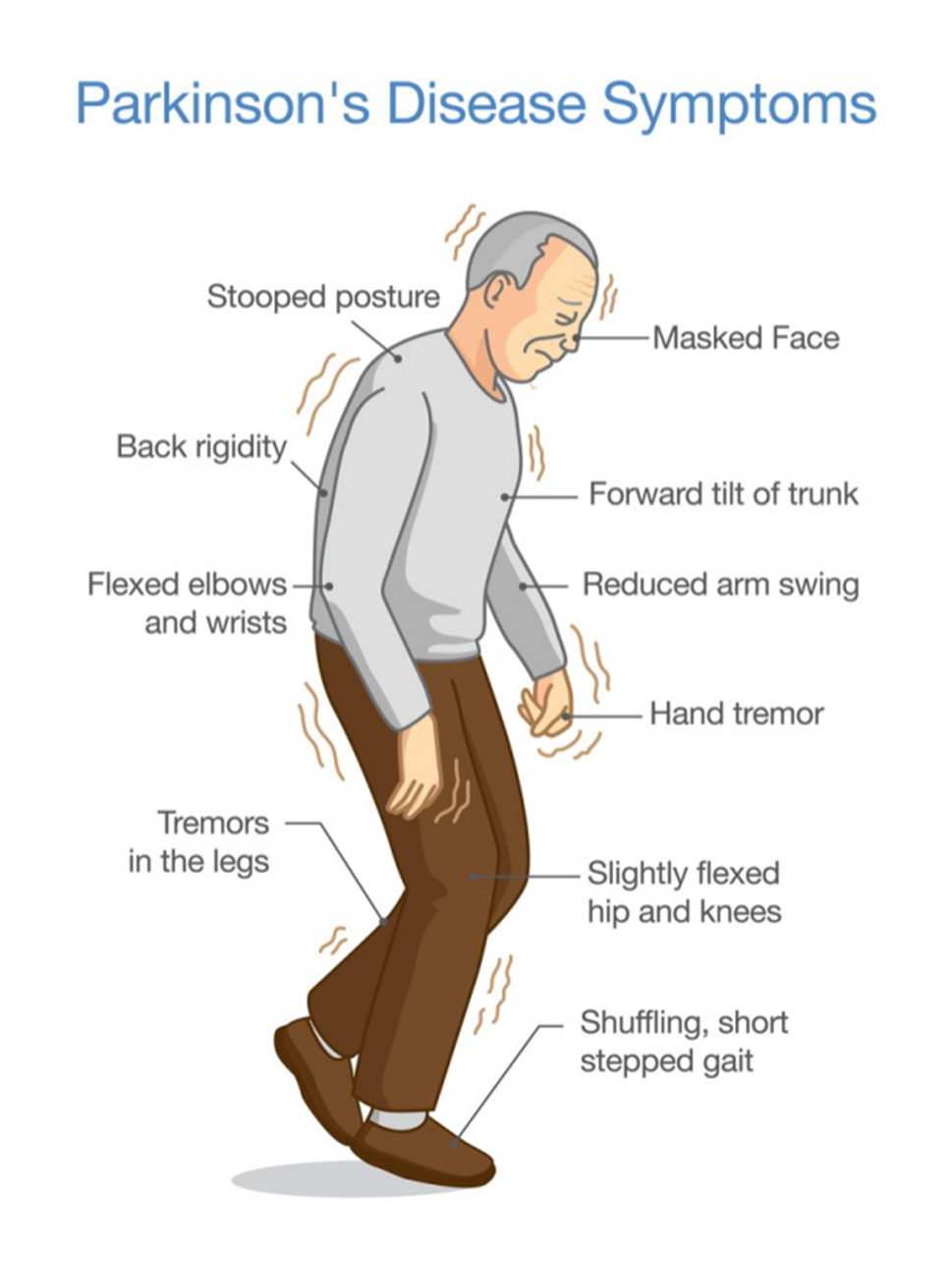
Telling his wife what the client needs is not the most effective discharge action. While it is important for the wife to understand the client’s needs, this approach is too passive and does not actively engage the client or his wife in the care process. Effective management of Parkinson’s disease requires active participation from both the client and the caregiver to ensure adherence to the care plan and to address any concerns or preferences they may have.
Choice B Reason:
Setting up visitations by a home health nurse can be beneficial, but it is not the most effective discharge action on its own. Home health nurses can provide valuable support and monitoring, but the success of the management plan also depends on the involvement and commitment of the client and his wife. Without their active participation, the care plan may not be fully effective.
Choice C Reason:
Involving the client and his wife in developing a plan of care is the most effective discharge action. This approach ensures that both the client and his wife are fully engaged in the care process, understand the management plan, and are more likely to adhere to it. Collaborative care planning allows for the consideration of the client’s and caregiver’s preferences, needs, and concerns, leading to a more personalized and effective care plan. This active involvement can also empower the client and his wife, improving their confidence in managing the disease.
Choice D Reason:
Writing up a detailed plan of care according to standards is important, but it is not the most effective discharge action if done in isolation. A standardized care plan may not address the unique needs and preferences of the client and his wife. Without their involvement in the development of the plan, there may be a lack of understanding or commitment to the care plan, reducing its effectiveness. Personalizing the care plan through active involvement of the client and his wife is crucial for successful management.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
