A nurse is teaching a client who reports taking gingko biloba to improve his memory. Which of the following adverse effects should the nurse include in the teaching?
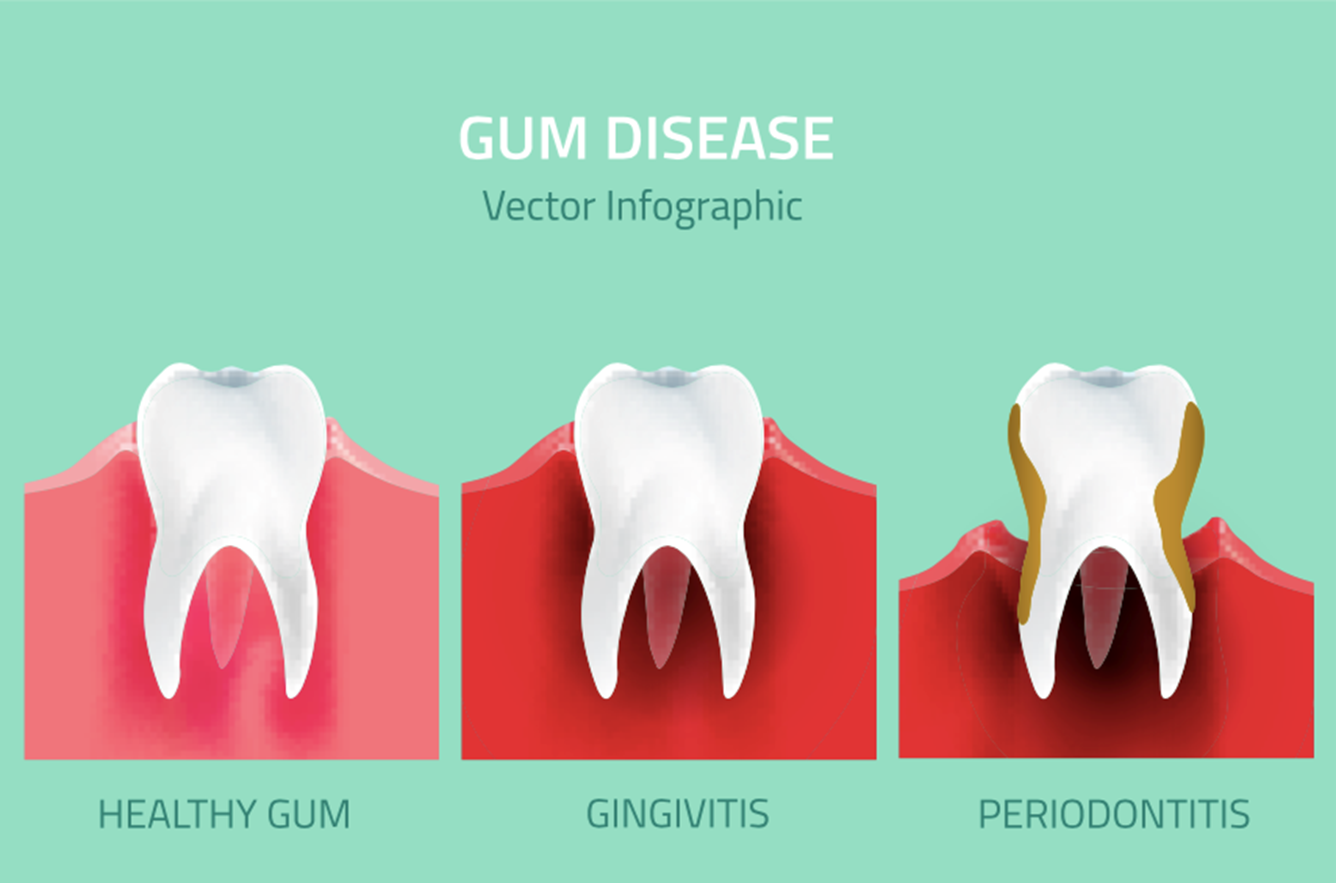
Bleeding gums
Decreased alertness
Breast enlargement
Bad breath
The Correct Answer is A
Choice A reason: Bleeding gums is a possible adverse effect of taking gingko biloba, as it may increase the risk of bleeding by inhibiting platelet aggregation and interfering with clotting factors. Gingko biloba may also interact with other medications that affect bleeding, such as anticoagulants, antiplatelets, or NSAIDs. The nurse should advise the client to monitor for signs of bleeding, such as bruising, nosebleeds, or hematuria, and report them to the provider.
Choice B reason: Decreased alertness is not a likely adverse effect of taking gingko biloba, as it may have the opposite effect of enhancing cognitive function and memory. Gingko biloba may improve blood flow to the brain and protect against oxidative stress and neuronal damage. The nurse should inform the client that gingko biloba may take several weeks to show its benefits and that the evidence for its effectiveness is inconclusive.
Choice C reason: Breast enlargement is not a known adverse effect of taking gingko biloba, as it does not affect the hormonal levels or the breast tissue. Gingko biloba may have some estrogenic activity, but it is not significant enough to cause gynecomastia or breast tenderness. The nurse should assess the client for other possible causes of breast enlargement, such as medications, liver disease, or tumors.
Choice D reason: Bad breath is not a common adverse effect of taking gingko biloba, as it does not affect the oral hygiene or the digestive system. Gingko biloba may have a mild odor, but it is not unpleasant or persistent. The nurse should advise the client to maintain good oral care and to check for other possible causes of bad breath, such as infections, dental problems, or dietary factors.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
The correct answer is: d. The client uses garlic to lower cholesterol levels.
Choice A: The client follows a low-fat diet to reduce cholesterol
Following a low-fat diet to reduce cholesterol does not have a significant impact on the effects of warfarin. While diet can influence overall health and cholesterol levels, it does not directly interact with warfarin’s anticoagulant properties.
Choice B: The client drinks a glass of grapefruit juice every day
Grapefruit juice is known to interact with various medications by inhibiting the cytochrome P450 enzymes, particularly CYP3A4. However, grapefruit juice does not significantly affect warfarin metabolism. It is more commonly associated with interactions with statins and other medications.
Choice C: The client sprinkles flax seeds on food 1 hr before taking the anticoagulant
Flax seeds are rich in omega-3 fatty acids and fiber, which can be beneficial for heart health. However, there is no strong evidence to suggest that flax seeds significantly potentiate the effects of warfarin. They do not have a direct interaction with the anticoagulant properties of warfarin.
Choice D: The client uses garlic to lower cholesterol levels
Garlic is known to have antiplatelet properties, which can enhance the anticoagulant effects of warfarin. This can increase the risk of bleeding in clients taking warfarin. Garlic can interfere with the blood clotting process, making it a significant factor to consider when managing a client on warfarin.
Correct Answer is D
Explanation
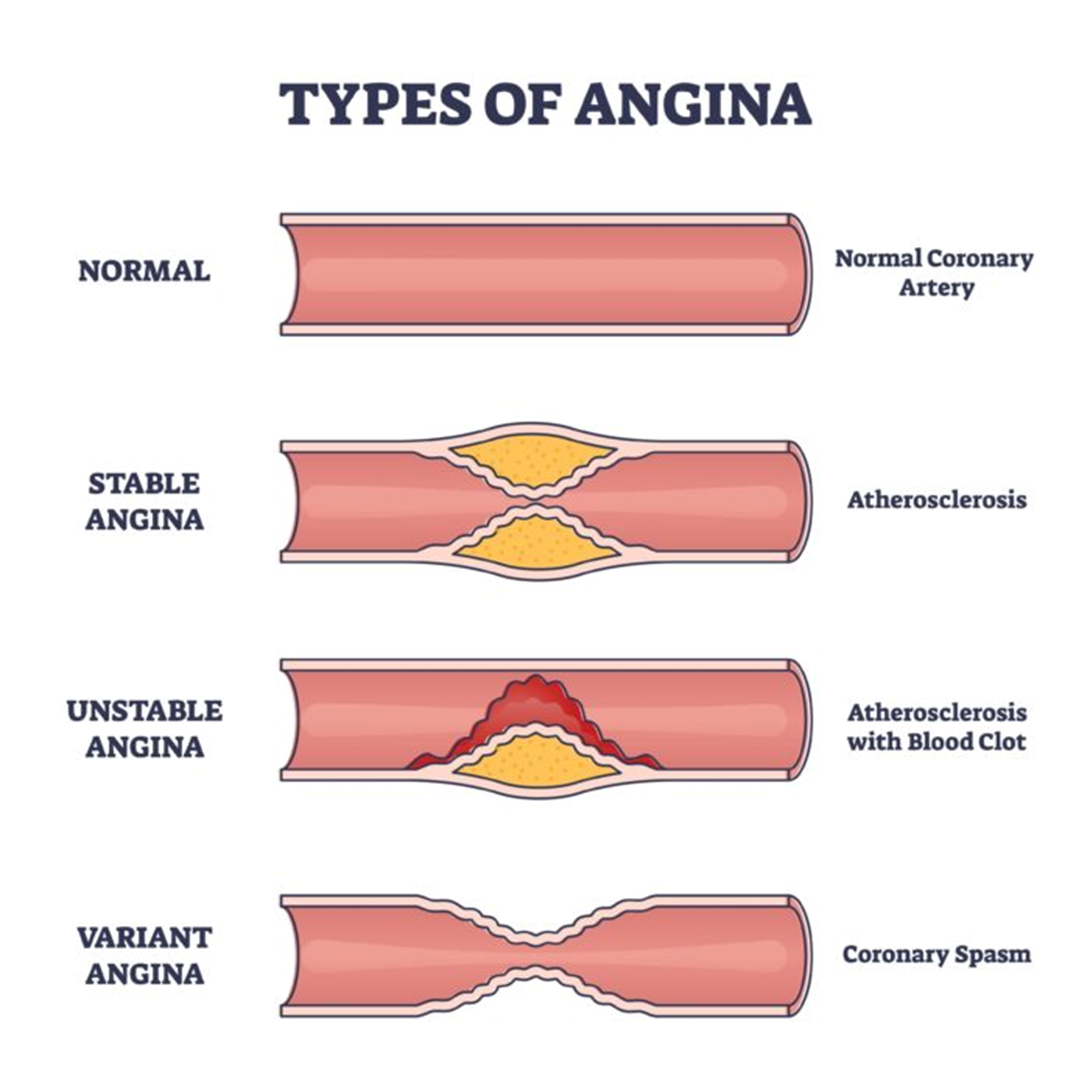
Choice A reason: "Place one tablet under your tongue every 5 minutes for 30 minutes to relieve chest pain." is not the correct statement. This is an incorrect and potentially dangerous instruction, as it can cause overdose and severe hypotension. The nurse should instruct the client to place one tablet under the tongue at the first sign of chest pain, and repeat every 5 minutes for up to three doses, if needed. The client should call 911 if the pain is not relieved after the first dose.
Choice B reason: "Nitroglycerin decreases chest pain by dissolving blood clots that are occluding the arteries." is not the correct statement. This is a false and misleading explanation of how nitroglycerin works. Nitroglycerin does not dissolve blood clots, nor does it affect the occlusion of the arteries. Nitroglycerin is a vasodilator that relaxes the smooth muscle of the blood vessels, especially the veins. This reduces the preload and the oxygen demand of the heart, and relieves the chest pain caused by ischemia.
Choice C reason: "You can store the bottle of tablets in your bathroom medicine cabinet." is not the correct statement. This is an inappropriate and unsafe storage recommendation, as it can affect the potency and effectiveness of the medication. The nurse should instruct the client to store the bottle of tablets in a cool, dry, and dark place, away from heat, moisture, and light. The client should also keep the bottle tightly closed and replace it every 6 months, or as directed by the provider.
Choice D reason: "Nitroglycerin dilates cardiac blood vessels to deliver more oxygen to the heart." is the correct statement. This is a simple and accurate description of how nitroglycerin helps to relieve anginal pain. Nitroglycerin dilates the coronary arteries, which supply blood and oxygen to the heart muscle. This improves the blood flow and oxygen delivery to the ischemic areas of the heart, and reduces the pain and discomfort.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
