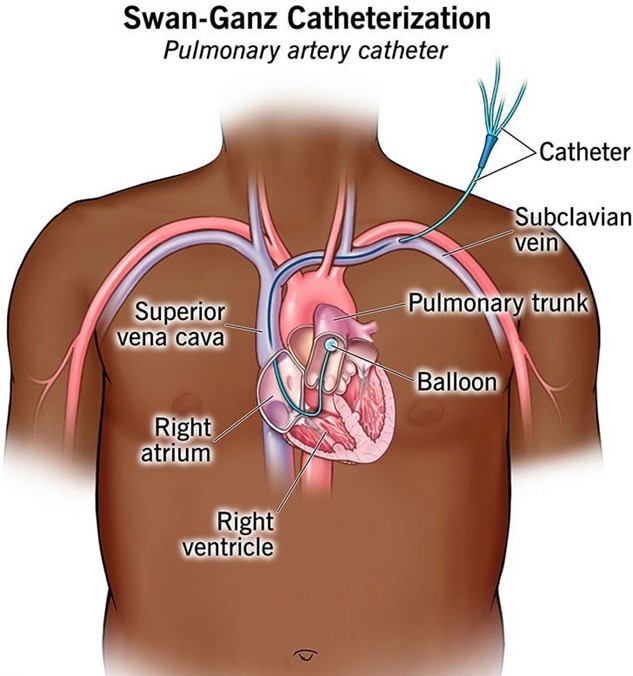
A nurse is preparing a client for transfer to the ICU for placement of a pulmonary artery catheter. The nurse should explain to the client that this catheter is used to monitor which of the following conditions?
Hemodynamic status
Spinal cord perfusion
Renal function
Intracranial pressure
The Correct Answer is A
Choice A Reason: This is correct because a pulmonary artery catheter is a device that measures the pressures and flows in the heart and lungs, such as the pulmonary artery pressure, the pulmonary artery wedge pressure, the cardiac output, and the mixed venous oxygen saturation. These parameters reflect the hemodynamic status of the client, which is the balance between the cardiac output and the systemic vascular resistance.
Choice B Reason: This is incorrect because a pulmonary artery catheter does not measure spinal cord perfusion, which is the blood flow to the spinal cord. Spinal cord perfusion can be affected by spinal cord injury, spinal anesthesia, or spinal surgery.
Choice C Reason: This is incorrect because a pulmonary artery catheter does not measure renal function, which is the ability of the kidneys to filter waste products and maintain fluid and electrolyte balance. Renal function can be assessed by urine output, blood urea nitrogen, creatinine, and glomerular filtration rate.
Choice D Reason: This is incorrect because a pulmonary artery catheter does not measure intracranial pressure, which is the pressure inside the skull. Intracranial pressure can be increased by brain injury, stroke, tumor, infection, or hydrocephalus.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Choice A Reason: Packed RBCs are indicated for clients who have hypovolemic shock due to blood loss, as they increase the oxygen-carrying capacity of the blood and restore the blood volume.
Choice B Reason: Cryoprecipitates are indicated for clients who have hemophilia or von Willebrand disease, as they contain clotting factors that help stop bleeding.
Choice C Reason: Albumin is indicated for clients who have hypovolemic shock due to fluid loss, such as from burns or ascites, as it increases the plasma oncotic pressure and draws fluid into the vascular space.
Choice D Reason: Platelets are indicated for clients who have thrombocytopenia or platelet dysfunction, as they help prevent or control bleeding.
Correct Answer is ["24"]
Explanation
- To find the concentration of heparin in the solution, divide the amount of heparin by the volume of D5W: 25,000 units / 500 mL = 50 units/mL
- To find the infusion rate, divide the prescribed dose by the concentration: 1,200 units/hr / 50 units/mL = 24 mL/hr
- Round the answer to the nearest tenth/whole number: 24 mL/hr
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
