A nurse is caring for a client who has preeclampsia and is being treated with magnesium sulfate IV. The client's respiratory rate is 10/min and deep-tendon reflexes are absent. Which of the following actions should the nurse take?
Prepare for an emergency cesarean birth.
Discontinue the medication infusion.
Place the client in Trendelenburg's position.
Assess maternal blood glucose.
The Correct Answer is B
Choice A) Prepare for an emergency cesarean birth is incorrect because this is not a priority or appropriate action for a nurse who is caring for a client who has preeclampsia and is being treated with magnesium sulfate IV.
Preeclampsia is a condition that causes high blood pressure, proteinuria, and edema during pregnancy. It can lead to complications such as eclampsia, which is seizures, or HELLP syndrome, which is hemolysis, elevated liver enzymes, and low platelets. Magnesium sulfate is a medication that helps to prevent or treat seizures in preeclamptic clients by relaxing the muscles and nerves. However, it can also cause side effects such as respiratory depression, hypotension, or loss of reflexes. Preparing for an emergency cesarean birth may be necessary if the client has severe preeclampsia or fetal distress, but it does not address the immediate problem of magnesium toxicity. Therefore, this action should be done only when indicated by the physician and after stabilizing the client's condition.
Choice B) Discontinue the medication infusion is correct because this is a priority and appropriate action for a nurse who is caring for a client who has preeclampsia and is being treated with magnesium sulfate IV. Discontinuing the medication infusion can help to stop or reduce the adverse effects of magnesium sulfate, such as respiratory depression, hypotension, or loss of reflexes. These effects can indicate magnesium toxicity, which is a life-threatening condition that can cause cardiac arrest or coma. The nurse should also notify the physician and prepare to administer calcium gluconate, which is an antidote for magnesium toxicity. Therefore, this action should be done as soon as possible for clients who show signs of magnesium overdose.
Choice C) Place the client in Trendelenburg's position is incorrect because this is not a safe or suitable action for a nurse who is caring for a client who has preeclampsia and is being treated with magnesium sulfate IV.
Trendelenburg's position means lying on the back with the head lower than the feet. It is sometimes used to improve blood flow to the brain or heart in cases of shock or hypotension. However, it can also cause complications such as increased intracranial pressure, decreased lung expansion, aspiration, or acid reflux. Moreover, it does not help to reverse or prevent the side effects of magnesium sulfate, such as respiratory depression, hypotension, or loss of reflexes. Therefore, this action should be avoided or used with caution for clients who are receiving magnesium sulfate IV.
Choice D) Assess maternal blood glucose is incorrect because this is not a relevant or necessary action for a nurse who is caring for a client who has preeclampsia and is being treated with magnesium sulfate IV. Blood glucose is the level of sugar in the blood that provides energy to the cells. It is measured by a blood test or a finger stick test. It can be affected by various factors such as diet, exercise, medication, or pregnancy. Assessing maternal blood glucose may be important for clients who have diabetes or gestational diabetes, which are conditions that cause high blood sugar levels that can harm the mother and the baby. However, it does not relate to preeclampsia or magnesium sulfate, which are conditions that affect blood pressure and nerve function. Therefore, this action should be done only when indicated by the physician and according to the client's history and needs.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Choice a) Placenta previa is incorrect because this is a condition where the placenta partially or completely covers the cervix, which can cause painless vaginal bleeding in the third trimester. It is not related to trauma and does not require hospitalization unless bleeding occurs.
Choice b) Dehydration is incorrect because this is a condition where the body loses more fluid than it takes in, which can cause symptoms such as thirst, dry mouth, headache, fatigue, and dizziness. It is not a complication of pregnancy and can be prevented by drinking enough water and avoiding caffeine and alcohol.
Choice c) Gestational hypertension is incorrect because this is a condition where the blood pressure rises above 140/90 mmHg after 20 weeks of pregnancy, which can cause complications such as preeclampsia, eclampsia, and fetal growth restriction. It is not caused by trauma and can be managed by regular antenatal care and medication if needed.
Choice d) Abruptio placentae is correct because this is a condition where the placenta separates from the uterine wall before delivery, which can cause severe vaginal bleeding, abdominal pain, uterine contractions, and fetal distress. It is a life-threatening emergency that can be triggered by trauma and requires immediate delivery of the baby and treatment of shock and blood loss. Therefore, a woman who is 8 months pregnant and involved in a serious motor vehicle crash should be admitted to the hospital for observation for this complication.
Correct Answer is D
Explanation
Choice a) They are born before 38 weeks of gestation is incorrect because this is not the definition of SGA. SGA refers to newborns who have a birth weight or length that is significantly lower than expected for their gestational age, regardless of when they are born. Therefore, a newborn can be SGA even if they are born at term or post-term.
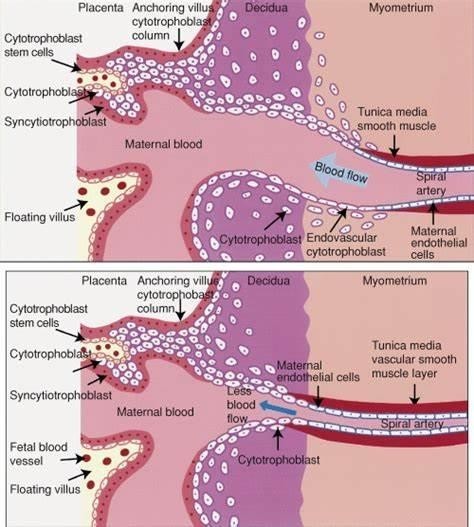
Choice b) Placental malfunction is the only recognized cause of this condition is incorrect because this is not the only factor that can contribute to SGA. Placental malfunction can cause fetal growth restriction due to insufficient blood supply and nutrients to the fetus, but there are other possible causes such as maternal factors (e.g.,
hypertension, diabetes, smoking, malnutrition), fetal factors (e.g., chromosomal abnormalities, infections, congenital anomalies), and environmental factors (e.g., altitude, pollution, stress).
Choice c) They weigh less than 2500 g is incorrect because this is not the criterion for SGA. SGA is based on the comparison of the newborn's weight or length with the expected values for their gestational age, not on an absolute cutoff. Therefore, a newborn can be SGA even if they weigh more than 2500 g, as long as they are below the 10th percentile for their gestational age.
Choice d) They are below the 10th percentile on gestational growth charts is correct because this is the most commonly used definition of SGA. Gestational growth charts are tools that plot the expected weight or length of a fetus or newborn according to their gestational age and sex. They are based on population data and can vary
depending on the ethnicity and region of origin of the mother and the baby. A newborn who falls below the 10th percentile on these charts is considered SGA, meaning that they have grown less than 90% of their peers .
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
