What is low birth weight classified as?
Weight is less than the 10th percentile (SGA)
Weight is greater than 90th percentile
Weight is between 10th and 90th percentile
Weight of 2500g or less at birth
The Correct Answer is D
Choice A: This is incorrect because weight less than the 10th percentile (SGA) means that the infant is smaller than expected for the gestational age, but not necessarily low birth weight. SGA infants may have intrauterine growth restriction due to maternal, placental, or fetal factors, but they may also be constitutionally small. SGA infants are at risk for hypoglycemia, hypothermia, polycythemia, and perinatal asphyxia.
Choice B: This is incorrect because weight greater than the 90th percentile means that the infant is larger than expected for the gestational age, but not necessarily high birth weight. Infants with weight greater than the 90th percentile are called large for gestational age (LGA) or macrosomic. LGA infants may have maternal diabetes, genetic factors, or post-term pregnancy as causes, but they may also be constitutionally large. LGA infants are at risk for birth trauma, shoulder dystocia, hypoglycemia, and respiratory distress.
Choice C: This is incorrect because weight between the 10th and 90th percentile means that the infant is appropriate for the gestational age (AGA), but not necessarily normal birth weight. AGA infants have a weight that matches their gestational age and are considered healthy and well-nourished. However, some AGA infants may have low or high birth weight depending on their gestational age at birth.
Choice D: This is the correct answer because low birth weight (LBW) is defined as a weight of 2500g or less at birth, regardless of the gestational age. LBW infants may be preterm (born before 37 weeks of gestation), term (born between 37 and 42 weeks of gestation), or post-term (born after 42 weeks of gestation). LBW infants are at risk for infection, bleeding, jaundice, and neurodevelopmental problems.

Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
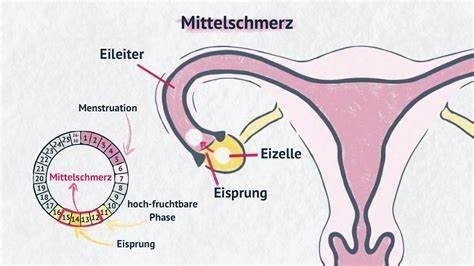
Choice a) A phase of the female menstrual cycle that involves the release of an egg (ovum) from one of the ovaries is incorrect because this is not the definition of Mittelschmerz, but rather the definition of ovulation. Ovulation is the process by which one or more eggs are released from the ovaries and travel to the fallopian tubes, where they can be fertilized by sperm. Ovulation usually occurs around the middle of the menstrual cycle, which is typically 28 days long, but can vary from person to person. Ovulation can be detected by changes in basal body temperature, cervical mucus, or hormone levels. Therefore, this response is inaccurate and misleading.
Choice B) A female reproductive organ in which ova or eggs are produced is incorrect because this is not the definition of Mittelschmerz, but rather the definition of ovary. The ovary is a paired organ that is located on either side of the uterus in the lower abdomen. The ovary contains thousands of follicles, which are sacs that contain immature eggs. Each month, one or more follicles mature and release an egg during ovulation. The ovary also produces hormones such as estrogen and progesterone, which regulate the menstrual cycle and pregnancy. Therefore, this response is irrelevant and inaccurate.
Choice C) The regular discharge of blood and mucosal tissue from the inner lining of the uterus through the vagina is incorrect because this is not the definition of Mittelschmerz, but rather the definition of menstruation. Menstruation is the process by which the endometrium, which is the tissue that lines the uterus and prepares for implantation of a fertilized egg, is shed and expelled through the vagina if pregnancy does not occur. Menstruation usually occurs once a month and lasts for about 3 to 7 days, but can vary from person to person. Menstruation can be accompanied by symptoms such as cramps, bloating, mood swings, or headaches. Therefore, this response is irrelevant and inaccurate.
Choice D) One-sided, lower belly pain associated with normal ovulation. Usually occurs about 14 days before the next menstrual period is correct because this is the definition of Mittelschmerz. Mittelschmerz is a German word that means "middle pain". It refers to a mild to moderate pain or discomfort that some women experience in their lower abdomen around the time of ovulation. The pain may last for a few minutes to a few hours and may switch sides from month to month depending on which ovary releases an egg. The pain may be caused by irritation or stretching of the ovarian or abdominal wall by the maturing follicle or by fluid or blood released during ovulation.
Mittelschmerz is not a sign of any disease or problem and does not require any treatment. However, it can be confused with other conditions that cause pelvic pain, such as appendicitis, ectopic pregnancy, or ovarian cysts. Therefore, women who have severe or persistent pain should consult their doctor for diagnosis and treatment. Therefore, this response is clear and accurate.
Correct Answer is C
Explanation
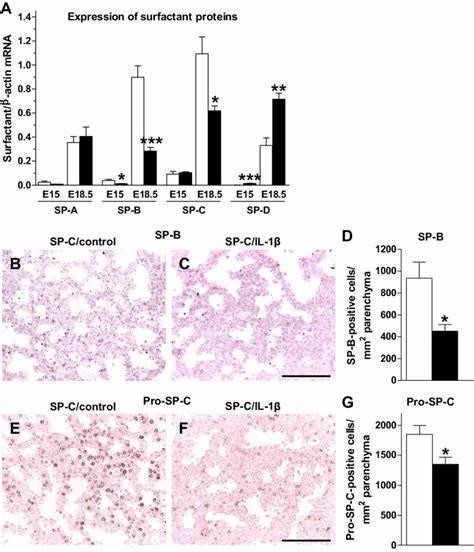
Choice A) dilates the bronchioles, decreasing airway resistance: This is not the correct function of surfactant.
Surfactant is a substance that reduces the surface tension of the fluid that lines the alveoli, which are the tiny air sacs in the lungs where gas exchange occurs. Surfactant does not affect the diameter of the bronchioles, which are the small airways that branch from the bronchi. Bronchodilation and bronchoconstriction are regulated by the autonomic nervous system and various mediators, such as histamine, epinephrine, and acetylcholine.
Choice B) provides transportation for oxygen to enter the blood supply: This is not the correct function of surfactant. Surfactant does not transport oxygen or any other gas. Oxygen diffuses from the alveoli into the capillaries, where it binds to hemoglobin in the red blood cells. The red blood cells then transport oxygen to the tissues via the blood circulation. Surfactant does not play a role in this process.
Choice C) keeps the alveoli open during expiration: This is the correct function of surfactant. Surfactant prevents the alveoli from collapsing during expiration by lowering the surface tension of the fluid that lines them. This allows for easier breathing and better gas exchange. Without enough surfactant, the alveoli tend to collapse and stick together, causing atelectasis, which is a condition where some or all of a lung collapses. Atelectasis can lead to hypoxia, respiratory distress, and infection.
Choice D) causes increased permeability of the alveoli: This is not the correct function of surfactant. Surfactant does not increase or decrease the permeability of the alveoli, which is the ability of substances to pass through them.
Permeability of the alveoli depends on several factors, such as pressure gradients, solubility, molecular size, and membrane thickness. Increased permeability of the alveoli can occur in conditions such as acute respiratory distress syndrome (ARDS), where fluid leaks into the alveolar space and impairs gas exchange. Surfactant does not cause this condition, but it can be affected by it.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
