Four hours after delivery of a healthy neonate of an insulin-dependent diabetic woman, the baby appears jittery, irritable, and has a high-pitched cry. Which nursing action has top priority?
Document the event in the nurses' notes.
Test for blood glucose level.
Notify the clinician stat.
Start an intravenous line with D5W.
The Correct Answer is B
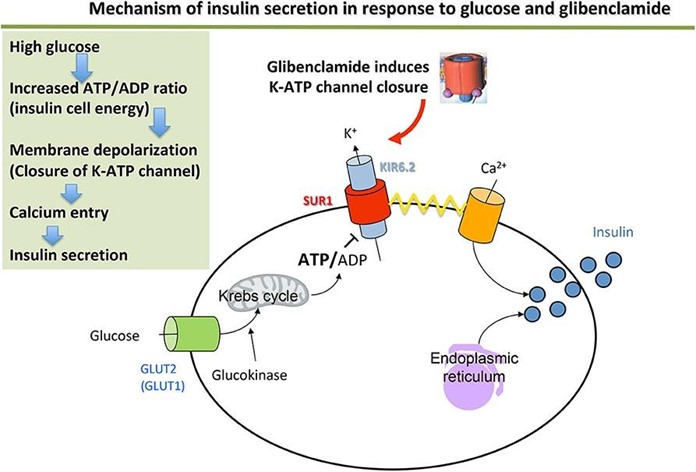
Choice a) Document the event in the nurses' notes is incorrect because this is not a priority action for a neonate who is showing signs of hypoglycemia. Hypoglycemia is a condition where the blood glucose level is lower than normal, which can cause neurological and metabolic problems in newborns. Neonates of diabetic mothers are at higher risk of developing hypoglycemia due to increased insulin production and decreased glycogen stores.
Documenting the event in the nurses' notes is an important step, but it should be done after assessing and treating the neonate's condition.
Choice b) Test for blood glucose level is correct because this is the most important action for a neonate who is exhibiting symptoms of hypoglycemia. The nurse should use a heel stick or a cord blood sample to measure the blood glucose level of the neonate as soon as possible, as hypoglycemia can lead to serious complications such as seizures, coma, brain damage, or death if left untreated. The normal blood glucose range for a full-term neonate is 40 to 60 mg/dL in the first hour of life, and 50 to 90 mg/dL thereafter. A blood glucose level below 40 mg/dL indicates hypoglycemia and requires immediate intervention.
Choice c) Notify the clinician stat is incorrect because this is not the most urgent action for a neonate who is suffering from hypoglycemia. The nurse should notify the clinician after confirming the diagnosis of hypoglycemia and initiating treatment, such as feeding or administering intravenous glucose. The clinician may order further tests or treatments depending on the severity and cause of the hypoglycemia, but the nurse should not delay the initial management of the neonate's condition.
Choice d) Start an intravenous line with D5W is incorrect because this is not the first-line treatment for a neonate who has hypoglycemia. D5W stands for dextrose 5% in water, which is a solution that contains glucose and water. It can be used to treat hypoglycemia by providing a source of energy and fluid to the neonate. However, before starting an intravenous line with D5W, the nurse should first attempt to feed the neonate with breast milk or formula, as this can also raise the blood glucose level and provide other nutrients and antibodies. If feeding is unsuccessful or contraindicated, then the nurse should start an intravenous line with D5W as ordered by the clinician.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is C
Explanation
Choice A) Newborns are abdominal breathers is incorrect because this is not a reason why the respiratory rate should be counted for a complete minute, but rather a characteristic of how newborns breathe. Abdominal breathing means that the diaphragm and the abdominal muscles are the main muscles used for breathing, rather than the chest muscles. Newborns are abdominal breathers because their chest wall is more compliant and less stable than adults, and their intercostal muscles are not fully developed. Abdominal breathing does not affect the accuracy or duration of measuring the respiratory rate, as long as the abdomen is visible and palpable. Therefore, this response is irrelevant and inaccurate.
Choice B) Activity will increase the respiratory rate is incorrect because this is not a reason why the respiratory rate should be counted for a complete minute, but rather a factor that can influence the respiratory rate. Activity means any physical or mental exertion that requires more oxygen and energy from the body. Activity can increase the respiratory rate, as well as the heart rate and blood pressure, to meet the increased oxygen demand and carbon dioxide removal. However, activity does not affect the accuracy or duration of measuring the respiratory rate, as long as the newborn is calm and resting during the measurement. Therefore, this response is irrelevant and inaccurate.
Choice C) The rate and rhythm of breath are irregular in newborns is correct because this is a reason why the respiratory rate should be counted for a complete minute. The rate and rhythm of breath refer to how fast and how regularly one breathes. Newborns have an irregular rate and rhythm of breath, which means that they breathe at different speeds and intervals, sometimes pausing for a few seconds between breaths. This is normal and harmless for newborns, as long as they do not stop breathing for more than 20 seconds or show signs of distress. However, it can make it difficult to measure the respiratory rate accurately, as counting for a shorter period may not reflect the true average rate. Therefore, counting for a complete minute can ensure a more reliable measurement. Therefore, this response is clear and accurate.
Choice D) Newborns do not expand their lungs fully with each respiration is incorrect because this is not a reason why the respiratory rate should be counted for a complete minute, but rather a feature of how newborns breathe.
Lung expansion means how much air one inhales and exhales with each breath. Newborns do not expand their lungs fully with each respiration, because they have smaller lung volumes and capacities than adults, and they breathe more shallowly and rapidly. However, lung expansion does not affect the accuracy or duration of measuring the respiratory rate, as long as the chest or abdomen movement is visible and palpable. Therefore, this response is irrelevant and inaccurate.

Correct Answer is D
Explanation
Choice a) Insert an indwelling urinary catheter is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Inserting an indwelling urinary catheter can cause trauma to the cervix or the placenta, which can worsen the bleeding and endanger the mother and the fetus. Therefore, this action should be avoided unless absolutely necessary.
Choice b) Prepare the abdominal and perineal areas is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Preparing the abdominal and perineal areas can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and obtaining informed consent for surgery.
Choice c) Witness the signature for informed consent for surgery is incorrect because this is not a priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery.
Witnessing the signature for informed consent for surgery can be done before performing a cesarean section, which is usually the preferred mode of delivery for placenta previa. However, this action should be done after stabilizing the client's condition and explaining the risks and benefits of surgery.
Choice d) Initiate IV access is correct because this is the priority action for a client who has a large amount of painless, bright red vaginal bleeding. This type of bleeding is suggestive of placenta previa, which is a condition where the placenta covers part or all of the cervix, preventing normal delivery. Initiating IV access can help to restore fluid volume, prevent hypovolemic shock, administer medications such as oxytocin or blood products if needed, and prepare for emergency cesarean section if indicated. Therefore, this action should be done as soon as possible to save the life of the mother and the fetus.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
